Did you know tight pants can increase your risk of urinary tract infections? Wearing overly snug clothing creates a warm, moist environment where bacteria thrive—making urinary tract infections (UTIs) more likely. If you've ever questioned your wardrobe’s impact on your urinary tract health, this comprehensive guide provides the clarity you need.

We dig into the scientific connection between tight clothing like skinny jeans or workout leggings and UTIs, revealing how your choices can protect or jeopardize your well-being. Discover actionable ways to prevent tract infections while maintaining both style and health.
Can Tight Pants Cause UTI? Understanding Urinary Tract Infections and Clothing Choices
The popular trend of wearing tight clothes—jeans, leggings, and form-fitting athletic gear—has raised new questions about how fashion impacts health. In particular, concerns about whether tight pants can cause urinary tract infections are becoming more common, especially among women and those who prefer tight clothes for fashion or fitness. In this article, we take a close look at the relationship between your clothing choices, urinary tract infection risk, and practical steps you can take to protect your health. With research-backed evidence and insights from healthcare professionals, you'll be equipped to make informed choices about what you wear and how it influences your urinary tract.
Wearing tight clothes may not be the sole cause of urinary tract infections, but it can certainly play a significant role in increasing UTI risk. The combination of warmth, moisture, and restricted airflow caused by snug garments creates an environment where bacteria such as Escherichia coli (E. coli) flourish. We’ll explain how this happens, break down common myths, and provide you with prevention strategies that go beyond just changing your wardrobe. By the end of this article, you’ll be empowered to enjoy the styles you love while keeping your urinary tract healthy.

What You'll Learn About: Can Tight Pants Cause UTI and Urinary Tract Health
The scientific connection between tight clothing and urinary tract infection risk
Main mechanisms by which tight pants can contribute to tract infections
Key prevention strategies focusing on clothing and hygiene
Common myths about tight clothes, yeast infections, and urinary tract infections debunked
What is a Urinary Tract Infection? The Basics on Urinary Tract and Tract Infections
Definition and Types of Urinary Tract Infections
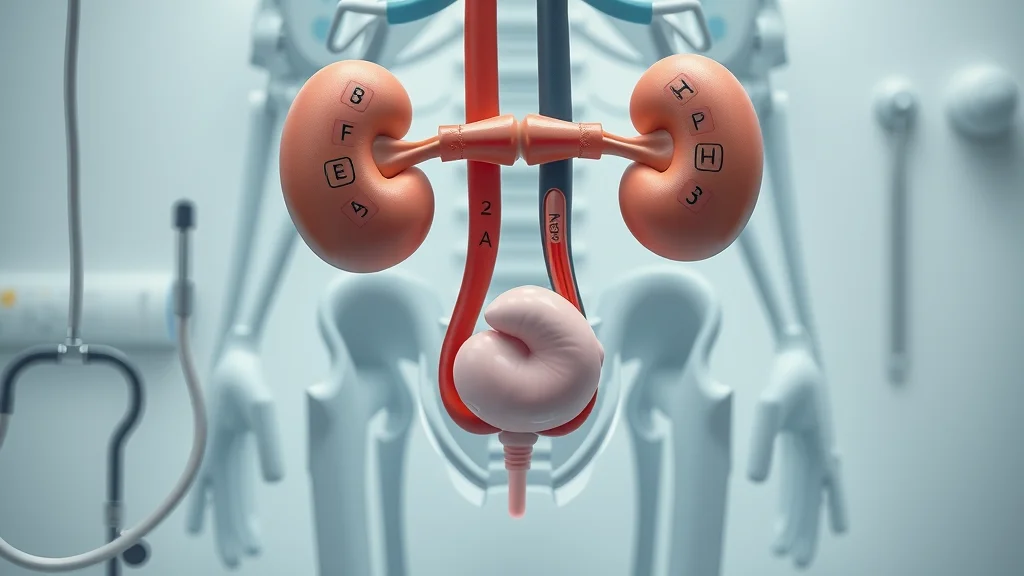
A urinary tract infection (UTI) is an infection that occurs in any part of the urinary system, including the kidneys, bladder, ureters, or urethra. Most UTIs develop in the lower part of the urinary tract—the bladder and urethra—but in some cases, infection can reach the kidneys and become more serious. UTIs are more common in women due to their anatomy, but men and children can also be affected.
There are several types of UTIs:
Cystitis (bladder infection): The most frequent type, characterized by inflammation of the bladder lining.
Urethritis (urethra infection): Infection and irritation of the urethra, the tube that carries urine outside the body.
Pyelonephritis (kidney infection): A serious infection of the kidneys, often resulting from untreated lower urinary tract infections.
Symptoms and Common Causes of Urinary Tract Infections
UTIs typically present with symptoms such as burning during urination, an urge to urinate frequently, cloudy or strong-smelling urine, pelvic pain, and—if left untreated—fever or back pain. In some cases, especially among the elderly or very young, symptoms may be mild or atypical, yet the risk of kidney involvement increases if not addressed. The most common causes of urinary tract infections include bacterial transfer from the rectum to the urethra (often by improper wiping—always wipe front to back), sexual activity, poor hygiene, certain contraceptive methods, and yes, tight clothing that traps moisture.
While the urinary tract has natural defenses, factors like wearing tight clothes, prolonged use of wet bathing suits, synthetic underwear, and poor hydration can set the stage for harmful bacteria to survive and multiply. Additionally, health habits such as not drinking enough water, delaying urination, or using irritating soaps further increase UTI risk. Understanding these triggers allows you to take proactive steps to safeguard your urinary tract health.
It's also worth noting that the impact of daily habits on your well-being extends beyond physical health. For example, exploring how positive routines like affirmations can support your overall wellness may complement your efforts to prevent infections. Learn more about the science behind affirmations and their role in boosting well-being in this evidence-based guide to affirmations and well-being.
How Tight Pants Can Cause UTI: Examining the Evidence on Tight Clothing
Can Wearing Tight Clothes Lead to Urinary Tract Infection?
The short answer: yes, wearing tight clothes significantly increases your risk of urinary tract infections by creating a warm, moist environment. Clothing that is overly snug restricts airflow and traps body heat and moisture, particularly in the genital region. This environment is a breeding ground for bacteria like E. coli, the main culprit behind most tract infections. When you wear tight jeans, workout gear, or underwear made from synthetic fabrics, you’re likely creating a space where bacteria can multiply quickly.
While UTIs have multiple causes, several studies and healthcare professionals have highlighted the link between tight clothing and an uptick in these infections. Individuals who regularly wear running tights, skinny jeans, or unbreathable undergarments—especially after sweating in workout gear or sitting in a wet bathing suit—are at even greater risk. The evidence suggests that making simple changes to your everyday clothing choices can play a major role in preventing unnecessary discomfort and potential health effects.

The Role of Moisture, Heat, and Bacteria with Tight Clothes
Moisture and warmth provide the perfect habitat for bacteria and yeast to flourish. When sweat and body heat are trapped by tight pants, leotards, or underwear, the microclimate in your genital area changes. Humidity cannot escape, leading to prolonged dampness—especially if you remain in wet or sweaty clothes after exercise or swimming. This build-up allows bacteria to migrate from skin or the rectum and climb up the urethra, increasing the risk for urinary tract infection.
In addition, tight clothing can cause small skin abrasions or irritation, disrupting the skin’s natural protective barrier. Microtears make it easier for bacteria to invade deeper tissues and reach the urinary tract. For those with sensitive skin or existing conditions like eczema, this risk is higher.
Wearing wet bathing suits for long periods, preferring tight clothes daily, or skipping regular clothing changes only adds to the problem. This is why medical professionals stress prompt changes after exercise or swimming and suggest opting for clothing made of breathable cotton.
Scientific Studies on Wearing Tight Pants and Tract Infection Risk
Recent research—including published studies in women’s health and primary care journals—confirms a significant correlation between tight clothing and an increased incidence of urinary tract infections. One study found that women who frequently wore tight pants or synthetic underwear experienced notably higher rates of both UTIs and yeast infections than those who wore looser, breathable garments. Scientists attribute this to greater skin-to-fabric friction, poor ventilation, and persistent moisture.
Notably, the risk rises in warm climates and among individuals with more active lifestyles. Surgeons and gynecologists interviewed in primary care settings consistently recommend avoiding tight clothing after intense workouts, swimming, and during hot weather. Additionally, research supports simple interventions like choosing looser pants and immediate post-workout clothing changes as highly effective in reducing UTI recurrence. While other contributors such as hydration, sexual habits, and hygiene remain vital, clothing is a modifiable factor within your control.
Comparison Table: Factors Contributing to UTIs |
||
Factor |
Impact on UTI Risk |
Prevention Tips |
|---|---|---|
Tight Clothing |
Traps heat and moisture, promotes bacterial growth |
Wear loose, breathable fabrics; change after sweating |
Poor Hygiene |
Allows transfer of bacteria from anus to urethra |
Wipe front to back; regular cleansing |
Hydration |
Low fluid intake increases infection risk |
Drink plenty of water; urinate regularly |
Sexual Activity |
Can introduce bacteria to urinary tract |
Urinate after intercourse; practice safe sex |
Wet Clothing |
Prolonged dampness fosters bacteria |
Avoid wearing wet bathing suits; change promptly |
Tight Pants, Yeast Infections, and Urinary Tract Infections: What's the Difference?
Can Wearing Tight Clothes Cause Yeast Infection or Yeast Infections?
Much like urinary tract infections, yeast infections can result from wearing tight clothes that trap moisture and heat. Yeast, especially Candida, thrives in warm, moist, and airless settings. When sweat and heat become trapped by leggings, tight underwear, or jeans, your natural skin flora is disrupted.
This tilts the balance in favor of yeast overgrowth, leading to symptoms like itching, burning, and thick discharge. While yeast infections and UTIs share some risk factors, they impact different areas: yeast infections affect the skin and mucous membranes (mostly the vagina for women), while UTIs involve the urinary tract.
It’s important not to confuse these two conditions. Many believe tight pants are a direct cause of both, when in reality, they simply create conditions that allow bacteria and yeast to flourish. Adopting smart hygiene habits—such as changing out of sweaty or wet bathing suits quickly, choosing breathable cotton underwear, and avoiding daily use of tight clothing—can reduce your risk of both yeast infections and UTIs. If symptoms persist or recur, consult a healthcare professional for proper diagnosis and care advice.

Other Risks of Wearing Tight Clothing: Beyond Tract Infections
Potential link between tight clothing and breast cancer (current research)
Impact of tight clothes on skin and general hygiene
General discomfort and long-term health effects
The dangers of wearing tight clothes extend far beyond urinary tract and yeast infections, including potential links to breast cancer. Some research is examining whether wearing tight clothes, such as tight bras or garments, could have links to breast cancer, although the evidence is currently inconclusive. Wearing tight clothes can also cause chafing, folliculitis, nerve compression, and other health effects such as poor circulation or reduced fertility in men. Poor hygiene and infrequent changing of sweaty clothing—often exacerbated by daily use of snug outfits or workout gear—are risk factors for additional skin infections and irritation.
It is vital to balance fashion preferences with comfort and overall health awareness. Making informed choices regarding both the fit and fabric of your clothes plays a significant role in minimizing everyday health risks.
"Wearing tight clothes can create an environment that promotes bacterial and yeast growth, which may increase the risk for urinary tract infections and yeast infections." – Medical Expert
How to Prevent UTIs When Wearing Tight Pants or Tight Clothing
Choose breathable fabrics and loose-fitting clothes whenever possible
Ensure proper personal hygiene and regular clothing changes
Stay hydrated to flush out the urinary tract
Avoid wearing wet or sweaty clothing for extended periods
Preventing urinary tract infections means taking simple, effective precautions with your wardrobe and daily habits. Select clothing made from natural fibers like cotton and linen, which allow the skin to breathe. Change out of sweaty gym clothes, wet bathing suits, or tight workout gear as soon as possible after use.
Practicing good hygiene—wiping front to back, washing regularly, and not using harsh soaps—protects your urinary tract, especially if you’re sensitive to frequent tract infections. Experts also recommend drinking cranberry juice and plenty of water daily to support urinary health. By understanding how tight clothing contributes to tract infection risk, you empower yourself to make confident, healthy choices.

People Also Ask: Your Questions on Can Tight Pants Cause UTI Answered
Can you get a UTI from tight undies?
Yes, wearing tight underwear—especially those made from synthetic fabrics—can increase your risk of urinary tract infections. Tight undies trap heat and moisture, fostering bacterial growth and making it easier for bacteria to migrate into the urinary tract. Opt for loose-fitting cotton underwear and change frequently for optimal protection.
What are the 8 most common causes of UTIs?
The most common causes of UTIs include: 1) poor personal hygiene (like not wiping front to back), 2) frequent sexual activity, 3) use of certain contraceptives such as diaphragms or lubricated condoms, 4) holding urine for long periods, 5) not drinking enough water, 6) diabetes or compromised immune system, 7) wearing tight clothes and synthetic underwear, and 8) prolonged use of wet bathing suits or sweaty workout gear.

Can wearing tight pants affect your bladder?
Yes, tight pants can put pressure on the lower abdomen and bladder. This extra pressure may increase the urge to urinate or contribute to bladder discomfort—even if a UTI is not present. Over time, it may exacerbate underlying conditions like interstitial cystitis or make urinary symptoms worse if you are already prone to tract infections.
Can tight pants cause infection?
Absolutely. Wearing tight pants—particularly if worn for long periods or when damp—can create the perfect conditions for both urinary tract infections and yeast infections. By trapping sweat and heat, these clothes encourage bacteria and yeast to multiply. Preventing infection requires choosing the right clothing, maintaining hygiene, and staying dry whenever possible.
Targeted FAQs: Can Tight Pants Cause UTI and Related Urinary Tract Questions
Does wearing tight clothing increase risk for urinary tract infection?
Are women more affected than men by tract infections from tight pants?
Can regular use of tight clothes cause recurrent tract and urinary tract infections?
Does wearing tight clothing increase risk for urinary tract infection?
Yes, medical studies indicate that tight clothing can trap heat and moisture, significantly raising the risk of UTIs, especially when combined with other risk factors like poor hygiene.
Are women more affected than men by tract infections from tight pants?
Yes, women’s anatomy makes them more susceptible to tract infections, and tight pants or underwear can amplify this risk by making bacterial transfer more likely.
Can regular use of tight clothes cause recurrent tract and urinary tract infections?
If you experience frequent UTIs, wearing tight clothing might be a contributing factor. Recurrent tract infections can often be reduced by switching to looser, natural-fiber clothing and improving hygiene routines.
Key Takeaways: Can Tight Pants Cause UTI? What You Should Remember
Wearing tight clothing, especially in warm and moist conditions, can increase the risk of urinary tract infection and yeast infections
Prevention is possible through clothing choices and hygiene
Consult a healthcare provider for recurrent tract infection symptoms
Conclusion: Rethink Tight Clothing to Protect Your Urinary Tract
Choose breathable, loose-fitting clothing and avoid wearing tight clothes to greatly reduce your UTI risk while staying stylish and comfortable.
Ready to upgrade your health and wardrobe? Discover best practices for urinary tract protection today.
As you continue to make informed choices for your physical health, remember that your overall well-being is shaped by many factors—including your mental and emotional state. If you’re interested in understanding how lifestyle changes, such as adjusting your wardrobe or daily habits, can also influence your mental health, take a deeper look at the broader impacts of isolation and self-care.
Our in-depth article on the hidden costs of isolation and its effects on mental health offers valuable insights and practical strategies to help you thrive in every aspect of life. Exploring these connections can empower you to build a holistic approach to wellness—one that supports both your body and mind for the long term.
Sources
CDC – https://www.cdc.gov/antibiotic-use/community/for-patients/common-illnesses/uti.html
NCBI – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6610441/
Women’s Health – https://www.womenshealth.gov/a-z-topics/urinary-tract-infections
Wearing tight clothing, such as skinny jeans or synthetic underwear, can create a warm, moist environment that promotes bacterial growth, potentially increasing the risk of urinary tract infections (UTIs). The Northern Inyo Healthcare District highlights that tight-fitting undergarments can trap moisture, allowing bacteria to multiply, and recommends opting for breathable fabrics like cotton to reduce this risk. (nih.org) Similarly,
The Women’s Health Clinic advises that tight clothing, especially synthetic underwear or trousers, can increase moisture and warmth in the genital area, promoting bacterial growth and potentially raising UTI risk. (thewomenshealth.clinic) By choosing loose-fitting, breathable clothing and maintaining good hygiene practices, you can help minimize the likelihood of developing UTIs.
 Add Row
Add Row  Add
Add 



Write A Comment