Sepsis affects over 1.7 million Americans annually, yet many don’t know how it starts. Understanding the hidden causes of sepsis is crucial for early detection and saving lives. Dive in to uncover the facts and protect yourself from this often overlooked medical emergency.
How Does Sepsis Happen? Understanding the Basics
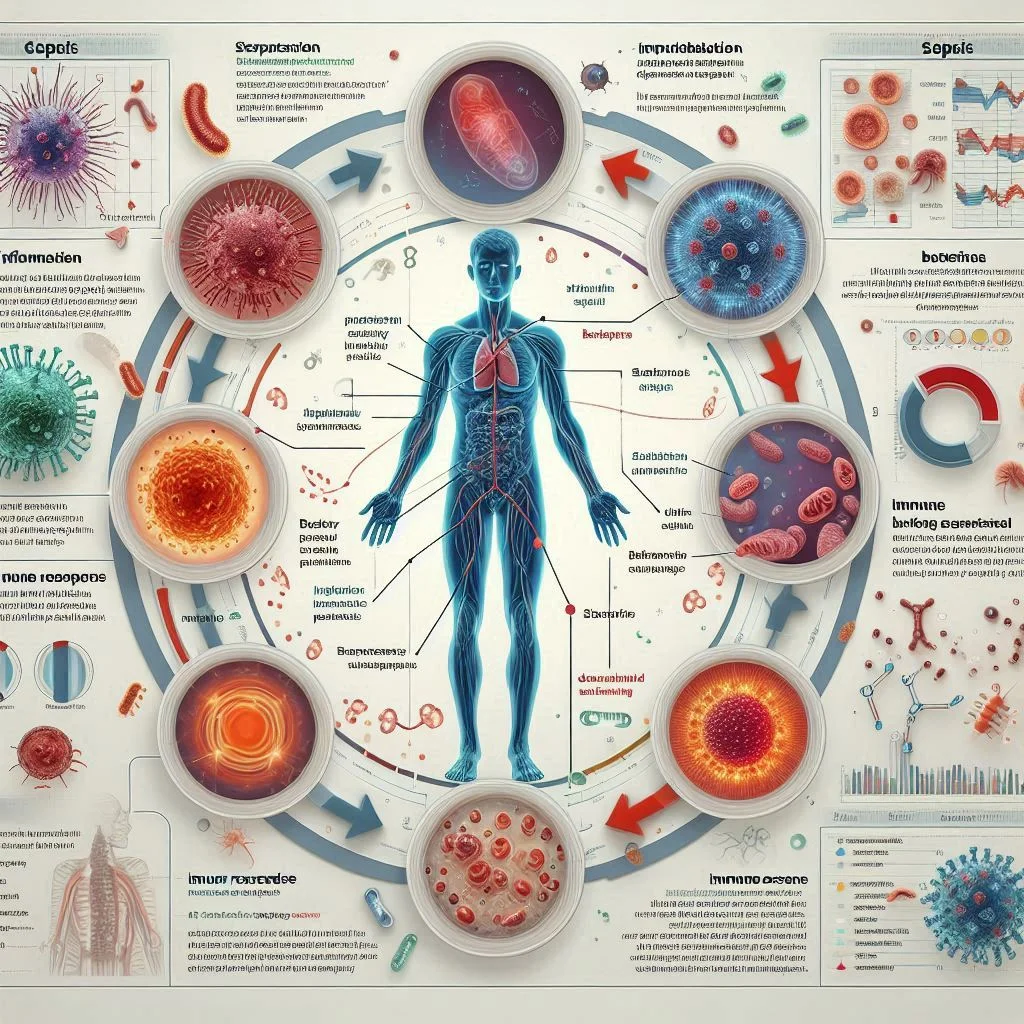
Sepsis is a rapid and potentially deadly medical emergency that occurs when your body's response to an infection spirals out of control, often leading to severe sepsis or septic shock if untreated. The immune system typically fights infections, helping you recover from minor illnesses swiftly. However, sepsis happens when this response is too aggressive, leading to widespread inflammation, damage to organs, and even death if not caught early. Many people view sepsis as something that strikes suddenly with little warning, but it often follows a logical—and preventable—sequence from infection to immune overdrive.
Searching for answers to how does sepsis happen? brings up medical terms like septic shock, severe sepsis, and organ failure. These terms point to the dangerous outcomes that develop if the underlying infection isn’t recognized and managed promptly. Whether originating from a bacterial infection, viral infections, or even fungal infections, sepsis doesn’t discriminate.
Understanding its roots can mean the difference between life and death—especially in vulnerable populations such as the elderly, those with chronic conditions, or anyone with a weakened immune system. Knowledge empowers quick action and could save your life or that of a loved one.
Sepsis: A Silent Medical Emergency
Sepsis is often referred to as a “silent” emergency because its early warning signs can be subtle or mistaken for other illnesses. By the time sepsis symptoms become obvious, a patient may already be in serious danger. The speed at which sepsis can escalate—from a mild infection to severe sepsis and even septic shock—makes it a race against time for both patients and healthcare providers.
One of the most critical aspects of sepsis is how quickly it can lead to organ damage, dangerously low blood pressure, and reduced blood flow to vital organs, escalating to severe sepsis or septic shock. If not managed in a timely manner, it may progress to multiple organ failure, requiring immediate medical intervention in an intensive care unit. Sepsis underscores the importance of expert care providers in early recognition and treatment, a subject we’ll explore throughout this guide.

Opening Hook: Why Knowing How Sepsis Happens Saves Lives
Recognizing the pathway of sepsis—how a simple infection can spiral into a life-threatening condition—arms you with the power to speak up, seek help, and potentially save lives. The difference between early intervention and delayed care often determines outcomes for people with sepsis. Fast action can prevent devastating complications, reducing the likelihood of organ damage and dramatically increasing survival chances.
By learning how sepsis happens, you make yourself an advocate for health—whether for a child with the flu, an elderly parent with a urinary tract infection, or for your own recovery after surgery. This guide breaks down each link in the chain from infection to recovery, so you can spot hidden danger and respond confidently.
While understanding the progression of sepsis is vital, it's equally important to recognize how your immune system's strength can influence your vulnerability to infections. For practical tips on supporting your immune health and potentially lowering your risk of severe complications, explore these evidence-based strategies to boost your immune system through nutrition and lifestyle.
What You'll Learn About How Sepsis Happens
A clear definition of how sepsis happens: Learn the fundamentals and sequence of events.
The step-by-step process by which sepsis starts: From minor infection to severe consequences.
Hidden causes and risk factors: Not just the obvious triggers, but rare and unexpected ones too.
Signs, symptoms, and how to act: What to watch for and when to seek help.
The relationship between infections and severe sepsis: How some germs are more dangerous than others.
Prevention and care provider insights: Tips and strategies to lower your risk of sepsis.
What Causes Sepsis to Start?
Answer: The role of infections and the body's immune response
Sepsis occurs when the body's immune system mounts an extreme response to an infection. It typically begins with a bacterial, viral, or fungal infection—such as pneumonia, urinary tract, skin, or abdominal infections. Instead of fighting the infection with precision, the immune system overreacts, flooding the bloodstream with chemicals that spark widespread inflammation. This chain reaction disrupts normal blood flow, causing blood clots and leaks within blood vessels.
As the inflammation spreads, the immune response meant to protect you starts causing severe harm: tissues can be damaged, organs can malfunction, and the whole body can enter a medical crisis condition. The unchecked inflammatory response is the pivot point—what starts as the body's natural defense quickly becomes the very process that places patients at higher risk of serious complications, even death, if not treated quickly by a care provider.
What is the Leading Cause of Sepsis?
Answer: Bacterial, viral infections, and severe sepsis explained
The majority of sepsis cases start with a bacterial infection, but viral infections and fungal infections can also trigger severe sepsis and septic shock. Common culprits include infections of the lungs (pneumonia), kidneys (urinary tract infections), abdomen, and skin wounds. These bacterial infections are often to blame because they can rapidly spread or become resistant to antibiotics, overwhelming the body's natural defenses.
However, viral infections and, less commonly, fungal infections can also lead to sepsis. High-risk viruses include influenza and, in some cases, COVID-19—especially in vulnerable populations. When the immune system is compromised by these infections, or when germs grow unchecked, the process can turn ordinary illnesses into full-blown medical emergencies. Regardless of the origin, any infection that triggers uncontrolled inflammation can progress to severe sepsis—and, without quick intervention, to septic shock or multiple organ failure.
Can Sepsis Be Caused by Poor Hygiene?
Answer: How hygiene impacts infection risk and triggers sepsis
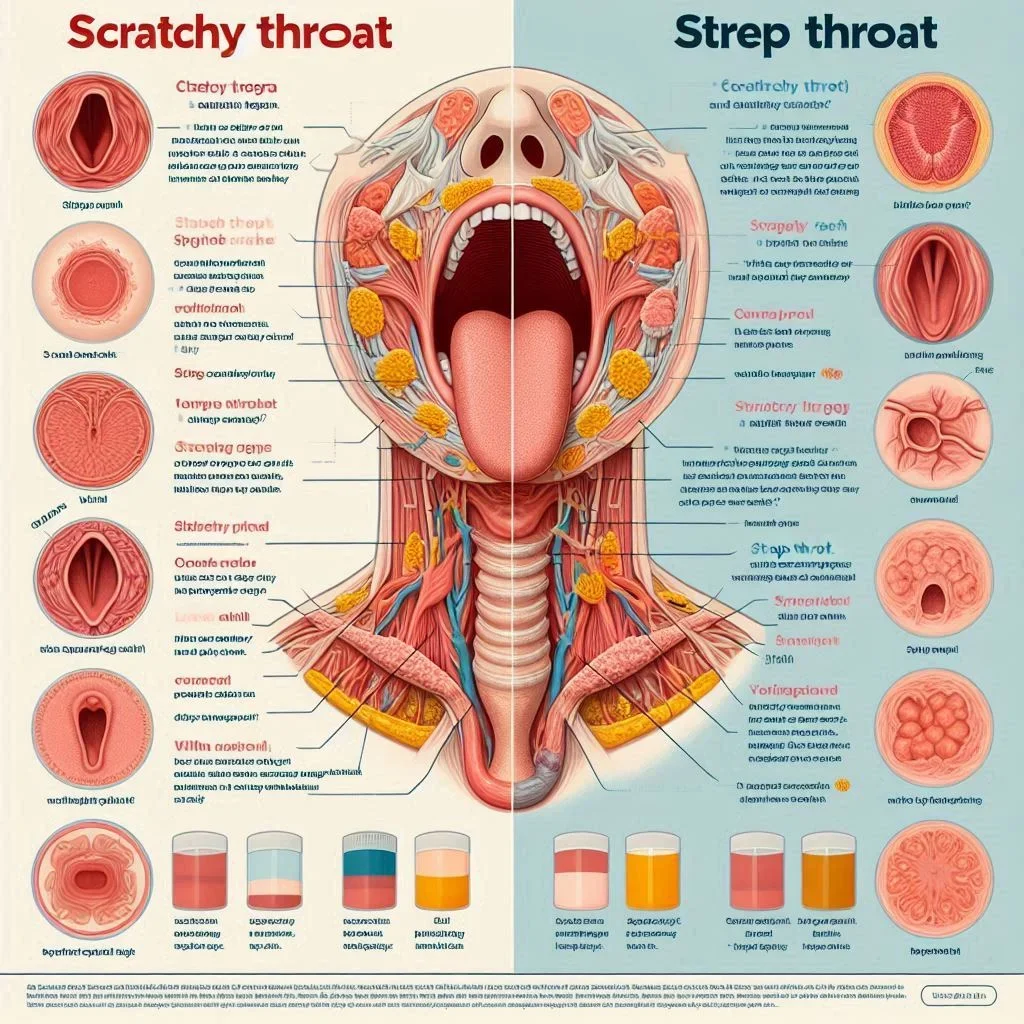
Poor hygiene can significantly increase your chance of infections that can lead to sepsis, including viral infections that may escalate to severe sepsis or septic shock. When bacteria or viruses enter the body through unwashed hands, contaminated surfaces, or untreated wounds, the risk of developing an infection rises sharply. In settings like hospitals or care units, where patients often have weakened immune systems, maintaining strict hygiene is especially vital to prevent the spread of pathogens.
For individuals at home, everyday habits like routine handwashing, cleaning cuts promptly, and ensuring a clean environment can act as your frontline defense. Even basic tasks—such as caring for a catheter or post-surgical wound—require careful hygiene. These prevention steps are your best bet against the types of bacteria and viruses that might otherwise slip past the immune system and start the dangerous spiral toward sepsis.

How Do You Avoid Sepsis?
Answer: Prevention strategies and the role of care providers
Preventing sepsis starts with stopping infections before they start or escalate, with care providers emphasizing early detection of symptoms of sepsis and monitoring blood pressure closely. Hand hygiene tops the list, but other crucial strategies include staying up-to-date on vaccinations (like flu and pneumonia shots), promptly treating skin wounds, and managing chronic illnesses. For high-risk patients, such as those in the intensive care unit, care providers follow strict protocols to limit catheter-related and surgical site infections.
At home, empowering yourself with knowledge—about when a routine infection could require urgent medical care—is equally essential. If you or someone in your care develops sudden symptoms of infection, especially when paired with confusion, shortness of breath, or rapidly dropping blood pressure, seek immediate help from a care provider. Regular medical check-ups and open communication with your healthcare team can greatly improve your ability to recognize and respond to infection risks early, reducing your chances of developing sepsis.
How Does Sepsis Happen? The Sequence from Infection to Septic Shock
From Mild Infection to Severe Sepsis: Pathophysiology Overview
To grasp how does sepsis happen, it helps to picture it as a chain reaction that can quickly progress from mild infection to severe sepsis and septic shock if blood pressure drops dangerously low. First, a mild infection occurs—perhaps a cut, urinary tract infection, or even pneumonia. Typically, the immune system deals with the invader and the threat passes. However, if germs enter the bloodstream, or the body’s defenses falter, the response can become uncontrollable. Chemicals released to fight the infection trigger widespread inflammation, jeopardizing healthy tissues and interfering with blood flow.
This escalating inflammation can damage the blood vessels, causing leaks and blood clots that inhibit blood flow to organs like the kidneys, heart, or brain. The situation then transitions to severe sepsis, marked by evidence of organ failure—such as difficulty breathing or decreased urine output. Without rapid intervention, sepsis can advance to septic shock, a life-threatening failure marked by plummeting blood pressure that is resistant to normal fluids and requires aggressive medical care.

Septic Shock: What Happens When Blood Pressure Crashes
In septic shock, the situation has reached a critical tipping point where blood pressure falls dangerously low, requiring immediate intervention by skilled care providers. The inflammation has caused such severe disruption to the blood vessels that blood pressure drops dangerously low, and blood can’t adequately reach vital organs. Medical staff may rush to administer IV fluids and medications to try to restore blood flow. Patients in septic shock often require care in an intensive care unit and may be at high risk for organ failure.
This phase is a true medical emergency. Immediate attention from a skilled care provider is necessary to prevent permanent organ damage or death. Sepsis treatment at this stage often includes potent antibiotics, intravenous fluids, blood pressure support, and sometimes machines to help with breathing or dialysis if organ systems begin to fail.
Watch:
Hidden and Emerging Causes: The Surprising Triggers for Sepsis
Viral infection and rare viral infections: Sepsis can begin from common viruses like influenza or more unusual, emerging illnesses.
Chronic diseases and increased risk: Conditions such as diabetes, cancer, or chronic kidney disease weaken defenses, making sepsis more likely.
Compromised immune systems and care provider insight: Patients on immunosuppressive medications, those with HIV/AIDS, or elderly individuals rely on astute healthcare teams to recognize sepsis early.
“Sepsis can begin with something as mundane as a small cut or a mild illness, underscoring the importance of vigilance,” — Infectious Disease Specialist
Common Symptoms of Sepsis and Early Warning Signs
Symptoms of sepsis everyone should know include fever or very low temperature, confusion, rapid breathing or heart rate, shivering, and other key symptoms of sepsis that require urgent medical attention.
When to consult a care provider: Any sudden, severe symptoms after infection warrant urgent medical attention, particularly in vulnerable groups.
How blood pressure changes signal severe sepsis: A noticeable drop in blood pressure may be the first sign of septic shock.

Risk Factors: Who Is Most Vulnerable to Sepsis?
Elderly patients
People with chronic illnesses
Individuals with compromised immune systems
Hospitalized individuals — especially in intensive care
Table: Comparing Causes and Triggers of Sepsis
Cause/Trigger |
Bacteria |
Viral Infections |
Hygiene Issues |
Chronic Disease |
|---|---|---|---|---|
Likelihood to Cause Sepsis |
High |
Moderate |
Indirect (increases infection risk) |
Increases vulnerability |
Examples |
Pneumonia, UTIs, wound infection |
Influenza, COVID-19 |
Poor wound care, lack of handwashing |
Diabetes, cancer, CKD |
Key Prevention |
Prompt antibiotics |
Vaccination, good care |
Hygiene practices |
Septic Shock and Severe Sepsis: Complications and Outcomes
Why blood pressure monitoring is vital in septic shock
Monitoring blood pressure is crucial when caring for people with sepsis because dangerously low blood pressure readings are the hallmark of septic shock and signal the need for immediate care provider intervention. Early detection of blood pressure changes enables care teams to intervene with lifesaving measures, such as IV fluids and medications to support the heart and blood vessels. This rapid action can be the key to survival and prevent irreversible organ damage or failure.
Frequent blood pressure checks are a standard in both hospital and home settings—especially for those who are elderly, critically ill, or in the intensive care unit. Small shifts may signal developing sepsis, making it essential for care providers and loved ones to act on these warning signs immediately.

Long-term impacts on recovery
Surviving sepsis or septic shock is only the beginning of a long recovery for many individuals. Organ damage sustained during the crisis can have lasting effects on mobility, cognition, and daily function. Some patients may require ongoing care or rehabilitation due to lingering weakness, chronic pain, or complications like heart failure or kidney disease.
Early and aggressive treatment of sepsis improves the odds of regaining independence, but family members, healthcare teams, and the patients themselves should prepare for possible long-term health management. Community support and specialized rehabilitation can greatly improve quality of life after severe sepsis.
Watch:
The Role of Care Providers in Sepsis: Early Diagnosis and Treatment
Best practice guidelines for early intervention: Hospitals and clinics use a checklist approach to screen for sepsis, checking vital signs, symptoms, and lab findings at first suspicion.
Common treatments (antibiotics, IV fluids, blood pressure medications): The “sepsis bundle” of therapies can halt progression when started fast—sometimes within the critical first hour of recognition.
How Does Sepsis Happen? The Importance of Early Detection and Action
How quick response can prevent severe sepsis and septic shock
Immediate recognition of symptoms of sepsis and swift medical care by care providers are the most effective tools in fighting sepsis and preventing progression to severe sepsis or septic shock. When patients, families, or care providers act quickly—calling 911 or going to the hospital at the first sign of rapid deterioration—outcomes improve dramatically. Early sepsis treatment prevents widespread inflammation, reduces organ damage, and lowers mortality risk.
If you suspect sepsis—due to symptoms like confusion, difficulty breathing, low blood pressure, or unrelenting fever—don’t wait. Insist on being evaluated for sepsis risk, and work alongside health professionals to ensure aggressive action is taken.
"Early detection and immediate medical care save lives—know the warning signs of sepsis."
Frequently Asked Questions About How Sepsis Happens
Can sepsis only happen in hospitals?
No, sepsis can start anywhere—even at home—from any infection that triggers an overwhelming immune response. However, hospitalized and intensive care patients are at higher risk due to underlying illnesses and exposure to healthcare-associated infections.Is sepsis contagious?
The infections that cause sepsis can be contagious, but sepsis itself is not spread from person to person. Good hygiene and infection control limit risk.What is the difference between sepsis and septic shock?
Sepsis is the body’s extreme response to infection that causes tissue damage and organ failure. Septic shock occurs when low blood pressure and abnormal cellular metabolism lead to life-threatening organ failure.How does the immune system respond to sepsis?
The immune system overreacts, releasing massive amounts of chemicals and causing widespread inflammation that injures tissues and organs.Are viral infections as dangerous as bacterial ones in causing sepsis?
While bacterial infections are more commonly associated with sepsis, certain viral infections (like influenza or COVID-19) can also lead to severe sepsis, especially in vulnerable individuals.

Key Takeaways: How Does Sepsis Happen?
Sepsis often starts with common infections but escalates quickly
Both bacterial and viral infections can trigger sepsis
Recognizing symptoms and acting fast is essential
Care providers play a crucial role in prevention and recovery
Act Now: Learn How Sepsis Happens to Protect Yourself and Loved Ones
Empower yourself with knowledge about sepsis—know the symptoms, stay vigilant, and seek prompt medical attention at the first sign of trouble.
If you’re interested in taking a more holistic approach to your health and understanding how chronic conditions can influence your risk for serious complications like sepsis, consider exploring the connection between autoimmune diseases and overall wellness.
This in-depth guide on scleroderma symptoms and management offers valuable insights into how underlying health issues can impact your immune system and long-term resilience. By broadening your knowledge of related health topics, you’ll be better equipped to advocate for yourself and your loved ones—empowering proactive choices and fostering a stronger foundation for lifelong wellness.
Sources
NIGMS – https://www.nigms.nih.gov/education/fact-sheets/Pages/sepsis.aspx
Mayo Clinic – https://www.mayoclinic.org/diseases-conditions/sepsis/symptoms-causes/syc-20351214
Understanding how sepsis develops is crucial for early detection and treatment. The Mayo Clinic’s article, “Sepsis - Symptoms & causes,” provides a comprehensive overview of sepsis, detailing its symptoms, causes, and risk factors.
In addition, the Centers for Disease Control and Prevention (CDC) offers valuable insights in their resource, “About Sepsis,” which explains the body’s extreme response to infection and emphasizes the importance of prompt medical attention.
If you’re serious about understanding sepsis and its implications, these resources will equip you with essential knowledge to recognize and respond to this life-threatening condition. NCWellnessHub.com
 Add Row
Add Row  Add
Add 



Write A Comment