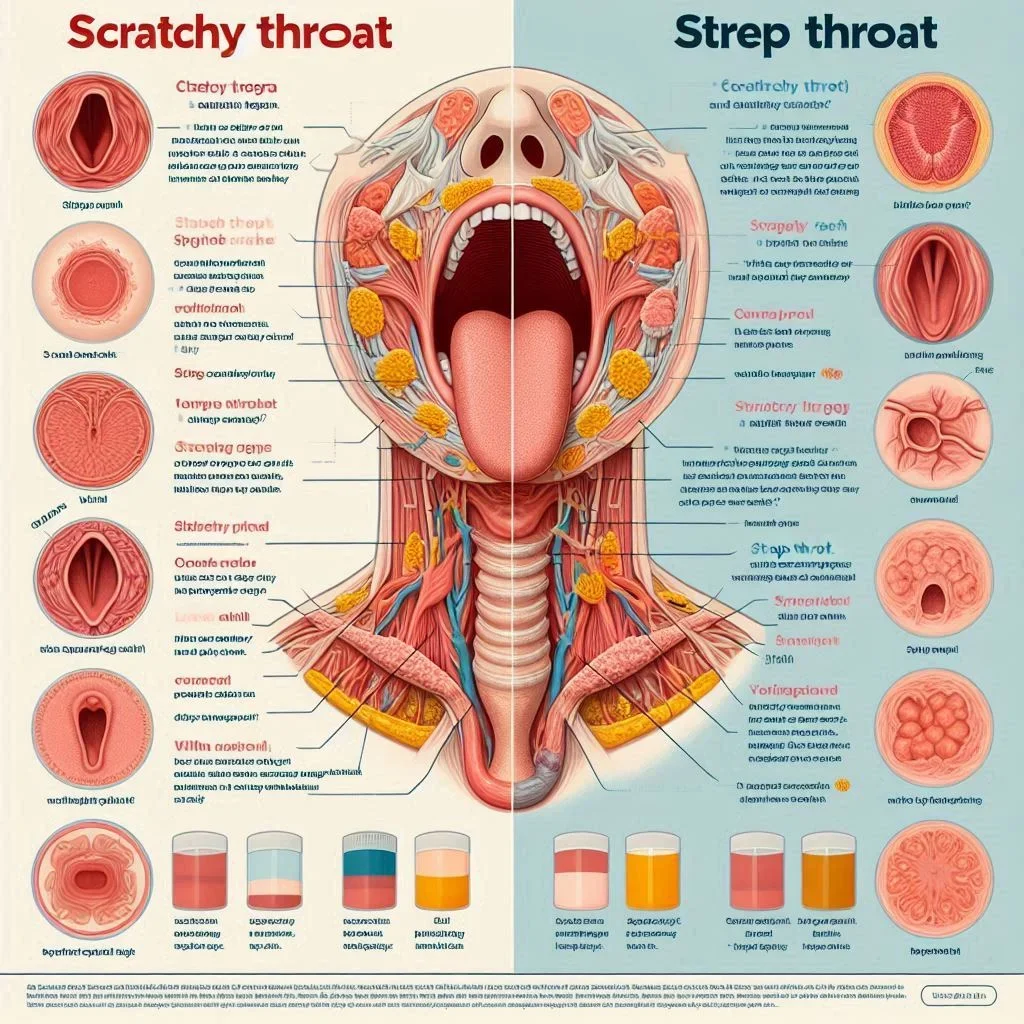
Is that scratchy throat just a cold, or could it be strep throat—a difference that could change your treatment? Understanding this key symptom helps you act faster and avoid complications. Let’s uncover the crucial clues doctors want you to know every winter.What You’ll Learn About Strep Throat Versus ColdKey differences between strep throat and the common coldThe crucial symptom that distinguishes sore throatsWhen to consult a healthcare provider or care providerEvidence-based insights from medical professionalsUnderstanding Strep Throat Versus Cold: Why One Symptom MattersOpening Hook: Key Facts About Strep Throat Versus ColdIs your sore throat just a common cold or actually strep throat? Critical differences to recognize early.Why accurate identification of cold and strep symptoms helps prevent complications."Many patients overlook the presence or absence of a cough, which is the one symptom most doctors rely on to distinguish a simple cold from strep throat." — Dr. Emily Nguyen, Family PhysicianStrep throat versus cold—a comparison that confuses so many people each winter. Both illnesses often start with a sore throat, leading families and individuals to wonder whether they’re facing a mild viral bug or a potentially serious bacterial infection. The single symptom that commonly separates the two conditions is the presence (or absence) of a cough. Understanding and recognizing this critical difference not only helps you manage sick days at home but may also prevent a missed diagnosis or dangerous complications—especially for kids and seniors.Expert insights, such as the guidance from Dr. Nguyen above, show just how important it is to act on warning signs with confidence. Whether you’re a parent looking out for a sick child or an adult monitoring your own health, knowing what distinguishes a cold and strep throat can keep you and your family safer throughout cold and flu season. Let’s explore the symptoms, causes, and care options that matter most.While understanding the subtle differences between strep throat and the common cold is essential, it's equally important to recognize how infections are targeted at the microbial level. For those interested in the science behind how certain medications work against bacterial threats, you might find it helpful to explore how DNA synthesis inhibitors like metronidazole combat infections—a topic that sheds light on why antibiotics are effective for some illnesses but not others.What Is a Sore Throat? Exploring Sore Throats in the Context of Common Cold and Strep ThroatDefining Sore Throat in Cold and Strep Throat CasesTypical causes of sore throatsComparison: sore throat in common cold, sore throat in strep throat"A sore throat with a runny nose and cough usually points to the common cold, not strep." — Dr. James Patel, ENT SpecialistA sore throat, also called pharyngitis, is among the most common upper respiratory symptoms seen in clinics and households alike. But not all sore throats are the same. Cold and strep throat cases both cause throat pain and discomfort, but they have different origins. The common cold is usually caused by a virus—such as rhinoviruses—and brings a scratchy or mildly painful throat, almost always accompanied by a runny nose, cough, and other upper respiratory symptoms.Symptoms of Strep Throat Versus Cold: The Key DifferencesCommon Symptoms in the Common Cold and Strep ThroatFever, sore throats, headache, runny noseThe symptoms of strep throat and the symptoms of a common cold share some overlap, leading to frequent misdiagnosis. Both illnesses may present with sore throat, mild fever, and headache, making it hard to distinguish at first glance. However, there are clear hallmarks that set them apart. In a common cold, the sore throat usually appears early and is less intense, while symptoms like a runny nose, persistent cough, and sneezing are almost always present. Cold symptoms typically start mild and progress gradually.In contrast, strep throat presents with a sudden, severe sore throat, high fever, and sometimes white patches or redness on the back of the throat and tonsils. Importantly, a cough and nasal symptoms are generally absent. Both can cause headaches and general malaise, but strep is more likely to trigger fatigue and difficulty swallowing. Remember: recognizing these distinctions can mean the difference between home care and seeking urgent medical attention for potential complications.SymptomCommon ColdStrep ThroatSore ThroatMild to moderate, scratchy, improves after 1-2 days, often with coughSevere, sudden onset, persists, worsens when swallowingFeverLow grade, rarely above 101°F (38.3°C)Frequently high, above 101°F (38.3°C), especially in childrenCoughCommon; often prominent throughout illnessRare or absentRunny NoseVery commonUncommon or absentHeadachePossible, not severeCommon, can be severeBody AchesMildModerate to severeRed or Swollen Throat/TonsilsSometimes mild rednessCommon; may see white patches, swollen tonsilsDuration5-10 days, symptoms gradually resolveImproves with antibiotics in 1-3 days, otherwise can persistThe One Symptom Doctors Say People MisreadThe presence or absence of coughSymptom progression: cold and strep throat timelines"If you have a severe sore throat without a cough, think strep, especially if accompanied by fever." — Dr. Linda Chen, Infectious Disease SpecialistMost people associate a sore throat with both the common cold and strep throat, but miss the single symptom that should guide their next steps: the cough. According to experts, a cough almost always comes with viral colds and rarely with strep throat. Parents often worry when a child complains of intense throat pain, but if that pain is not accompanied by a cough—and is coupled with fever or headache—it’s time to suspect strep and see a care provider.Symptom progression also offers clues: a cold starts with a gradual sore throat, then cough, then congestion and low-grade fever, peaking at day 3–5 before fading. Strep, on the other hand, often hits hard within hours, bringing a sudden sore throat, high fever, and difficulty swallowing. Recognizing these patterns and knowing when a cough is present—and, importantly, when it’s not—could change your treatment and prevent complications like rheumatic fever or kidney inflammation.The Science Behind Strep Throat Versus ColdWhat Causes Strep Throat and the Common Cold?Strep Throat: Streptococcus pyogenes bacteriaCommon Cold: Rhinoviruses & other virusesStrep throat is a classic example of a bacterial infection: specifically, it’s caused by Streptococcus pyogenes, also known as group A strep. This germ spreads via droplets from an infected person’s cough or sneeze, making close-contact environments like schools and families particularly vulnerable. Because it’s bacterial, strep throat responds well to antibiotics—but only if recognized promptly.The common cold, by comparison, is caused by a virus. Over 200 known viruses can cause cold symptoms, with rhinoviruses leading the pack. Viral infections are far more common than bacterial, and most sore throats in winter are actually due to viral causes. Crucially, antibiotics will not help with a cold and can contribute to antibiotic resistance if used unnecessarily. Understanding these causes is the backbone of good treatment decisions for sore throats, especially when you suspect strep throat.Transmission and Risk FactorsHow strep throat and common colds spreadHigh-risk groups for each conditionBoth strep throat and common cold spread primarily through respiratory droplets released when an infected person coughs, sneezes, or talks. You can contract the illness by close contact, touching contaminated surfaces, or sharing utensils. While anyone can get sick, children aged 5–15 are most at risk for group A strep infections, whereas adults and children alike frequently catch colds, especially during colder months and in crowded settings. Other risk factors for strep throat include recent exposure to a person with strep throat, weakened immune system, or existing respiratory conditions.Prevention remains similar for both: frequent handwashing, avoiding close contact with sick individuals, and not sharing utensils or drinks. Understanding how these illnesses spread helps prioritize public health measures, especially during outbreaks or in schools and offices.How Doctors Diagnose Strep Throat Versus ColdTests and Tools Healthcare Providers UseRapid strep testThroat culturesSymptom checklists for sore throats and the common coldDiagnosing strep throat versus cold begins with a thorough symptom checklist and history. Your healthcare provider will ask about the type and onset of symptoms, presence or absence of cough, and may physically examine the throat and tonsils for redness, swelling, or pus. The most definitive diagnostic tools include the rapid strep test—a quick swab test that detects group A strep antigens in minutes—and a throat culture, which can confirm infection over 1–2 days. These tests help limit unnecessary antibiotic use and provide peace of mind for parents and patients.Routine use of symptom checklists ensures common symptoms of cold and strep throat aren’t overlooked: severe sore throat, no or mild cough, rapid onset, and fever raise suspicion for strep, while prominent cough and runny nose point toward viral illness. Your care provider uses these clues, alongside objective tests, to make an accurate diagnosis and recommend next steps.Clinical Guidelines: When to See a Healthcare Provider or Care ProviderWarning signs and red flag symptomsWhen to seek immediate medical attentionThere are times when self-care at home is enough—and times when a visit to your care provider is necessary. Red flag symptoms for which you should seek medical attention include: sudden severe throat pain, difficulty swallowing or breathing, high fever persisting over 48 hours, drooling, rash, or swelling in the neck or face. If your sore throat is accompanied by symptoms such as chest pain, confusion, or inability to keep fluids down, call a healthcare provider or visit urgent care immediately.The role of your primary care provider is essential in evaluating persistent or severe sore throats. Early recognition and testing can prevent complications like rheumatic fever or post-strep kidney inflammation. When in doubt, always err on the side of caution and schedule an exam.Case Studies: Real-Life Examples of Strep Throat Versus ColdPatient story: Missed diagnosis leads to complicationsPatient story: Early identification and proper careOne recent example involved a 9-year-old who developed a severe sore throat but continued attending school, believing it was just another common cold due to her ongoing cough and mild fever. Her parents delayed seeking care, but after symptoms worsened and swallowing became more painful, they visited a healthcare provider. Testing confirmed strep throat—by then, she had developed signs of rheumatic fever, a preventable complication.Contrast this with a teen who, after experiencing sudden intense throat pain, absence of cough, and high fever, sought medical attention promptly. Thanks to early evaluation and a rapid strep test, he received antibiotics and recovered without complications. These stories highlight the difference timely recognition of strep throat versus cold can make in preventing long-term health risks.Treatment Options for Strep Throat Versus ColdTreating Strep Throat: Antibiotics and Supportive CarePrescription antibiotics for strep throatOnce a strep infection is confirmed, the most effective treatment of strep throat is a course of antibiotics such as penicillin or amoxicillin, prescribed by your healthcare provider. Antibiotics reduce the duration of symptoms, decrease infectiousness to others, and—crucially—prevent rare but serious complications like rheumatic fever or kidney inflammation. Supportive care (rest, hydration, throat lozenges, and over-the-counter medications for pain or fever) is essential for recovery and comfort.It’s important to complete the entire prescribed antibiotic course—even if you feel better—to ensure the bacteria are eradicated. This minimizes the risk of recurrent infection and reduces antibiotic resistance in the community.Managing the Common Cold: At-Home RemediesRest, fluids, over-the-counter medicationsWhy antibiotics don’t work for the common coldIf symptoms point to a common cold rather than strep throat, the focus shifts to supportive care at home. Best practices include getting ample rest, drinking plenty of fluids, and using over-the-counter remedies such as acetaminophen or ibuprofen for fever and pain. Warm tea, throat lozenges, and humidified air can relieve discomfort. Because colds are caused by a virus, antibiotics are ineffective and should not be used—doing so contributes to resistance and does not speed recovery.Symptoms of a cold typically resolve in 5–10 days. If symptoms worsen or new severe signs develop, consult a care provider to rule out secondary bacterial infections or other complications. Always stay home when experiencing fever or pronounced cold symptoms to prevent transmission to others.Preventing Complications in Sore ThroatsTaking swift, informed action when you suspect strep throat can prevent dangerous complications like rheumatic fever, post-streptococcal glomerulonephritis (a kidney disorder), or abscess formation. For the common cold, avoid unnecessary antibiotics, but do monitor for signs of secondary infections, especially in children and the elderly. Timely recognition and medical care are keys to a healthy recovery.Strep Throat Versus Cold: When to Call a Care ProviderSymptoms requiring urgent medical attentionRole of primary care providers and urgent care clinicsImmediate evaluation by a primary care provider or urgent care clinic is warranted if you (or your child) have trouble breathing or swallowing, persistent high fever, or neck swelling—especially in the setting of severe sore throat and absence of cough. These could signal strep throat or a complication that needs prescription treatment fast. If in doubt, prioritize your safety and call your doctor or clinic.Mild symptoms that do not worsen and fit the common cold profile can often be managed at home. Still, if symptoms do not improve in a week or if you have underlying medical conditions (like diabetes, immune suppression, or heart disease), speaking to a healthcare provider is always a good idea.How to Tell if Strep Throat or Cold? (People Also Ask)Strep often lacks cough but has fever and severe sore throat; colds typically include cough and runny nose with milder sore throat.To differentiate strep throat versus cold, use this quick checklist:Is your sore throat very painful with sudden onset, and is there no cough or runny nose? Suspect strep.Do you have a cough, congestion, and a mild sore throat that improves after a day or two? It’s likely a common cold.If in doubt, or if severe symptoms develop, see a healthcare provider for a strep test.What Does Day 1 of Strep Look Like? (People Also Ask)Day 1 of strep throat begins with sudden-onset sore throat, pain swallowing, fever, and possible headache—no cough or nasal congestion.The first day of strep throat usually features a sudden, severe sore throat, pain on swallowing, fever, and sometimes headaches or abdominal pain—especially in kids. Unlike a cold, strep rarely involves a cough or runny nose at the onset. A cold, by contrast, starts more mildly and gradually.Can Strep Cause Nosebleeds? (People Also Ask)Strep throat rarely causes nosebleeds directly, but severe throat irritation or forceful nose blowing during illness can contribute.While not a common symptom of strep throat, nosebleeds can sometimes occur during the illness due to aggressive nose blowing or dry, irritated nasal passages if the illness triggers mouth breathing or congestion. Rarely, untreated strep may cause blood vessel inflammation which can increase the risk of minor bleeds.Can Strep Throat Cause Swollen Cheeks? (People Also Ask)Swollen cheeks are uncommon in strep throat; if present, may signal complications or a different infection—see a healthcare provider immediately.Swelling of the cheeks may represent a complication (such as an abscess or a spreading infection), especially if accompanied by redness, fever, or difficulty opening the mouth. Typical strep infection does not cause facial swelling. Always consult a care provider if you experience this with a sore throat.Strep Throat Versus Cold: Key TakeawaysStrep throat versus cold often comes down to one overlooked symptom: coughTimely recognition and seeking care prevent complicationsConsult a healthcare provider if in doubt about symptomsFrequently Asked Questions about Strep Throat Versus ColdHow contagious is strep throat versus a common cold?Both spread easily in close quarters, but strep requires antibiotics to stop transmission, while you are most contagious with a cold at symptom onset. Both require careful hand hygiene and cough etiquette.What home remedies help relieve symptoms?Warm soups, throat lozenges, honey (not for infants), rest, and adequate fluids help relieve sore throats and speed recovery for both conditions.How long does each condition last?Colds typically last 5–10 days. Strep throat improves within 1–3 days of antibiotics but can persist or worsen if left untreated.What are the risks of untreated strep throat?Untreated strep can cause rheumatic fever, kidney issues, abscesses, and rarely life-threatening complications.Summary and Next Steps if You Suspect Strep Throat Versus ColdRecap of symptom checklistHow to monitor symptoms at homeWhere to get medical help if unsureIf you’re unsure, monitor your symptoms: track the presence or absence of cough, fever, and severity of sore throat. If symptoms fit strep or worsen, contact your healthcare provider for evaluation and possible rapid strep test.Get Professional Care if You Have Symptoms of Strep Throat Versus ColdBook an appointment or telehealth consult to confirm your diagnosis and get appropriate treatment today.ConclusionRecognize the signs, trust the checklist, and don’t hesitate to seek care—acting early makes all the difference when it comes to strep throat versus cold.If you’re committed to staying healthy through every season, it’s worth looking beyond just acute infections and considering how your daily habits impact your overall resilience. For example, quality sleep is a powerful ally for your immune system, helping your body fend off both viral and bacterial threats more effectively.To discover how getting the right amount of rest can sharpen your mind and strengthen your defenses, explore why prioritizing 7–9 hours of quality sleep is essential for brain and immune health. Small lifestyle upgrades can make a big difference in your ability to recover quickly and stay well all year long.SourcesCDC – Group A Strep – https://www.cdc.gov/groupastrep/diseases-public/strep-throat.htmlMayo Clinic – Strep Throat Symptoms – https://www.mayoclinic.org/diseases-conditions/strep-throat/symptoms-causes/syc-20350338Children’s Healthcare of Atlanta – Streptococcal Pharyngitis – https://www.choa.org/medical-services/infectious-diseases/streptococcal-pharyngitisNHS – Sore Throat – https://www.nhs.uk/conditions/sore-throat/CDC – Common Cold – https://www.cdc.gov/dotw/common-cold/index.htmlUnderstanding the differences between strep throat and the common cold is crucial for effective treatment and preventing complications.The article “Cold vs Strep: Differences, Symptoms, Treatments, and More” provides a comprehensive comparison, highlighting that colds are typically caused by viruses like the rhinovirus, while strep throat results from a bacterial infection by Streptococcus pyogenes. It emphasizes that both conditions are contagious and spread through respiratory droplets. (healthline.com)Also, the Cleveland Clinic’s article “Do You Have Just a Sore Throat or Is It Strep?” offers insights into distinguishing symptoms. It notes that a cough is common with viral sore throats but typically absent in strep throat cases. The piece also underscores the importance of seeking medical attention for a definitive diagnosis and appropriate treatment. (health.clevelandclinic.org)If you’re serious about accurately identifying and treating throat infections, these resources will provide you with the necessary information to make informed decisions. NCWellnessHub.com
 Add Row
Add Row  Add
Add 



Write A Comment