
Did you know that up to 50% of SIBO breath tests produce inaccurate results due to improper preparation? Many individuals unknowingly compromise their small intestinal bacterial overgrowth diagnosis by overlooking essential SIBO breath test preparation steps. Proper SIBO breath test preparation can make the difference between clarity and confusion in diagnosing small intestinal bacterial overgrowth and managing your digestive health. In this guide, you’ll master the essential preparation steps, avoid the most common pitfalls, and unlock accurate, actionable results from your hydrogen and methane breath tests.
Unlocking Accuracy: Why SIBO Breath Test Preparation Steps Matter
The journey to reliable hydrogen breath test and methane breath test results begins with diligent preparation. SIBO breath test preparation steps aren’t optional—they’re vital to detecting small intestinal bacterial overgrowth (SIBO) with confidence. Failure to carefully follow the prescribed guidelines can lead to misleading gas levels, false positives, or inconclusive outcomes. For individuals dealing with irritable bowel syndrome or other gut health concerns, this can delay the right diagnosis and effective treatment.
Prep errors such as consuming high-fiber foods, neglecting fasting requirements, or taking inappropriate medications may inadvertently alter hydrogen breath test and methane breath test results. By understanding and adhering to proper hydrogen breath test protocols, you empower your healthcare provider to get a clear picture of your intestinal bacterial composition. Following these steps ensures that your breath sample reflects the true state of your small intestine, not the aftermath of a meal or recent medications.
"Up to 50% of SIBO breath tests produce inaccurate results due to poor preparation—knowing the right steps makes all the difference."

Understanding the SIBO Breath Test and Breath Test Fundamentals
The SIBO breath test is a simple yet powerful diagnostic tool designed to accurately detect small intestinal bacterial overgrowth by measuring intestinal bacterial activity. At its core, this breath test measures the levels of hydrogen and methane gas in your breath after ingesting a sugar solution. Excessive bacteria in the small intestine ferment the sugar and produce these gases, which are then absorbed into the blood, transported to the lungs, and expelled in your breath sample. This process allows healthcare providers to evaluate the presence and severity of bacterial overgrowth with minimal discomfort and maximum insight.
There are two primary types of breath tests for SIBO: the hydrogen breath test and the methane breath test, both essential for assessing small intestinal bacterial overgrowth and intestinal bacterial imbalances. Each has unique roles in detecting different types of intestinal bacteria activity. The selection and interpretation of the breath test should always be guided by your healthcare provider, who will contextualize the results based on your specific symptoms and medical history. Understanding which test is right for you is part of the broader strategy for mastering SIBO breath test preparation steps.
For those interested in how digestive health conditions can impact broader wellness, it's worth noting that certain systemic diseases, such as AL amyloidosis, may also present with gastrointestinal symptoms. Understanding the overlap between gut health and systemic conditions can help you and your provider interpret breath test results within a larger health context.
How Breath Tests Detect Small Intestinal Bacterial Overgrowth
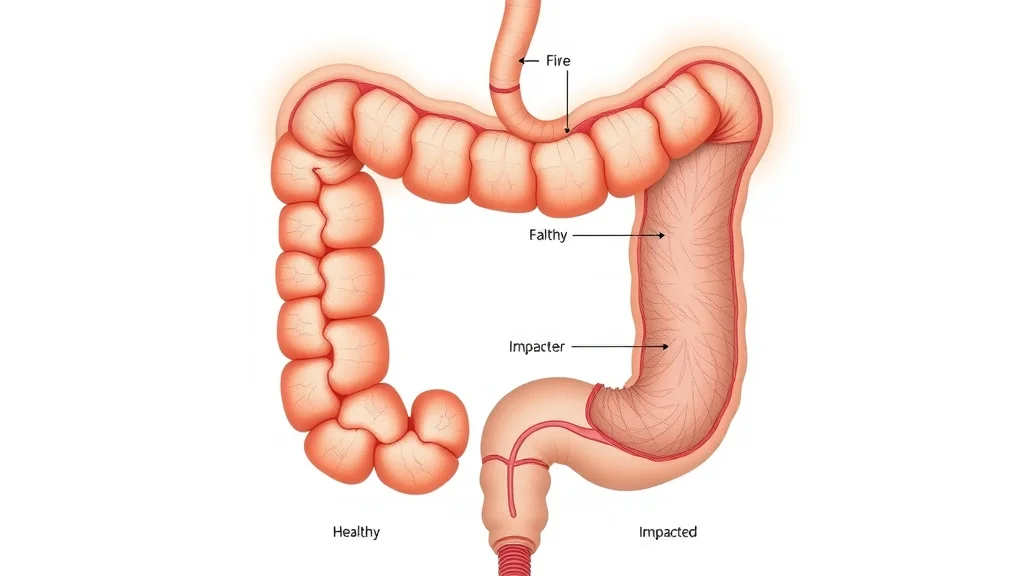
Small intestinal bacterial overgrowth occurs when intestinal bacteria, normally found in the large intestine, begin to colonize the small intestinal environment, disrupting normal bacterial balance. This bacterial overgrowth results in fermentation of ingested sugars, leading to the production of hydrogen and methane gases detected by breath tests. In a SIBO breath test, after fasting, you ingest a sugar solution such as lactulose or glucose. If excessive bacteria are present in the small intestine, they metabolize the sugar quickly and release detectable gases.
The gases produced—hydrogen and methane—are absorbed through the intestinal wall and transported via the bloodstream to the lungs, where they are exhaled and measured during the hydrogen breath test and methane breath test. Breath tests measure the concentration of these gases at specific intervals, which helps pinpoint whether bacterial overgrowth is occurring in the small intestine versus the large intestine. This method is non-invasive and highly specific for diagnosing gut bacterial imbalances, making strict adherence to SIBO breath test preparation steps all the more critical.
Hydrogen Breath Test vs. Methane Breath Test: Key Differences
Hydrogen breath tests and methane breath tests are related but serve slightly different functions. The hydrogen breath test is typically the first line of investigation, measuring the hydrogen gas produced by bacterial fermentation of a test sugar. However, some types of intestinal bacteria, such as methanogens, convert hydrogen into methane. This means that in some cases, a methane-only producing overgrowth can occur, resulting in low hydrogen readings but elevated methane.
By comparing results from both tests, healthcare providers obtain a more comprehensive view of small intestinal bacterial dynamics. In fact, many clinics now use combined hydrogen and methane breath tests for higher accuracy. Knowing which gases to measure and understanding your body's microbial composition can refine your SIBO diagnosis and guide effective treatments for both hydrogen and methane-dominant small intestinal bacterial overgrowth.
Comparison of Hydrogen Breath, Methane Breath, and SIBO Breath Tests
Test Type |
Measured Gases |
Accuracy |
Duration |
Primary Use Case |
|---|---|---|---|---|
Hydrogen Breath Test |
Hydrogen |
High for hydrogen-producing SIBO |
2–3 hours |
Detect hydrogen-producing bacteria overgrowth |
Methane Breath Test |
Methane |
High for methane-dominant SIBO (constipation type) |
2–3 hours |
Identify methanogen overgrowth |
Combined SIBO Breath Test |
Hydrogen & Methane |
Highest (dual detection) |
2–3 hours |
Most accurate for both types of small intestinal bacterial overgrowth |
Essential SIBO Breath Test Preparation Steps for Reliable Results
Thorough SIBO breath test preparation steps are non-negotiable for obtaining accurate and reliable hydrogen breath test and methane breath test results. Every aspect of preparation, from diet to fasting to medications, directly influences your breath test’s sensitivity and specificity. The aim is to minimize variables that could either spike or suppress hydrogen and methane gas production outside of bacterial metabolism. By adhering to a proven checklist, you dramatically increase the chances of a definitive diagnosis, providing your healthcare provider with the actionable data they need.
Being methodical in your approach to hydrogen breath test preparation ensures your breath samples accurately reflect the state of your small intestinal bacteria and intestinal bacterial overgrowth, rather than recent meals or other confounding factors. Many patients who prepare well discover that their test results align tightly with their gut symptoms, empowering a tailored approach to treating small intestinal bacterial overgrowth and restoring digestive health. Let’s get into the definitive steps for foolproof SIBO breath test preparation.
TL:DR
Follow a low-fermentation, low-residue diet for 24 hours prior to testing
Fast completely (no food or drink except water) for 12 hours before the test
Avoid all non-essential medications—check with your healthcare provider
Do not exercise or smoke for at least one hour before the test
Refrain from using mouthwash, chewing gum, or mints the night before and day of the test
Brush teeth the night prior, but don’t brush within two hours of the test
Dietary Guidelines Before the SIBO Breath Test: What to Eat and Avoid
Proper diet before your small intestinal bacterial overgrowth test dramatically influences gas production and sample accuracy. The 24 hours leading up to your SIBO breath test should feature simple foods that minimize fermentation and residue. Safe choices usually include plain white rice, eggs, baked or broiled chicken or fish (no seasoning), and small amounts of clear broth. Avoid all dairy, high-fiber foods, fruits, vegetables, whole grains, and sweeteners during this period. These items can feed excess intestinal bacteria and skew test results, leading to potential misdiagnosis or unnecessary treatments by your healthcare provider.
Tempting as it may be to snack or indulge in complex meals, adhering to these dietary restrictions ensures a true baseline for detecting irritable bowel or similar symptoms. The less fermentable substrate you provide prior to your hydrogen breath test, the clearer your provider can zero in on the presence and extent of small intestinal bacterial overgrowth. This disciplined approach is essential for maximizing the benefit of your SIBO breath test preparation steps.

The Importance of Fasting Before Your Hydrogen Breath Test
Fasting before your hydrogen breath test is a cornerstone of reliable sample collection. This means abstaining from all food and beverages (except water) for at least 12 hours before your SIBO breath test appointment. This overnight fasting period eliminates the chance of undigested material fermenting in the gut, a primary source of false positive gas readings. Healthcare providers emphasize that even a small meal or beverage can rapidly alter the hydrogen or methane output and confuse the test results, making it harder to diagnose actual intestinal bacterial overgrowth.
If you slip and eat or drink anything other than water during the fasting window, you should reschedule your small intestinal bacterial overgrowth test. The results may not be trustworthy, potentially delaying next steps and targeted treatment. Water is the only allowable intake, as it doesn’t interfere with fermentation or gas production, supporting the test's integrity. Commitment to this fasting protocol is one of the most important SIBO breath test preparation steps on your checklist.
Step-by-step walkthrough: SIBO Breath Test Preparation Steps Explained Visually
Common Mistakes That Jeopardize SIBO Breath Test Preparation Steps
Even the best-intentioned patients can inadvertently undermine their SIBO breath test by making avoidable mistakes. A primary source of error is neglecting to pause certain medications that alter gas levels or motility, such as antibiotics, probiotics, or laxatives. Always confirm with your healthcare provider before the test to determine which medications to temporarily suspend. Additionally, consuming foods or drinks that feed excessive intestinal bacteria in the 24 hours before the test can skew your hydrogen or methane results and mask real symptoms.
Timing mishaps—like late-night snacking, exercising, or even using strong mouthwashes—can confound your data and reduce test reliability. Personal diligence and careful review of the SIBO breath test preparation steps are the best safeguards against these pitfalls. It's critical to view these measures not merely as requirements, but as allies on your path to accurate, actionable diagnosis with your healthcare team.
Avoiding Bacterial Overgrowth Confounders During Breath Tests
Avoiding external confounders is essential for ensuring that your hydrogen breath test reflects the actual small intestinal environment. This means refraining from activities or substances that could alter the results, such as smoking, chewing gum, or taking certain supplements or over-the-counter remedies. Even minor deviations, like consuming coffee or using cough drops, might introduce enough variables to either falsely elevate or suppress gas levels, skewing the medical interpretation.
One commonly overlooked confounder is incomplete medication review. Medications like antibiotics can suppress existing bacteria, whereas probiotics or antifungal treatments may artificially alter the balance of your gut flora. Creating a detailed, up-to-date list of medications and supplement intake for your healthcare provider ensures that your approach is as thorough as possible. This careful attention keeps the test focused solely on detecting true small intestinal bacterial overgrowth.

Medication and Lifestyle Factors Affecting Small Intestinal Breath Test Outcomes
In addition to food and water, lifestyle factors play a significant role in SIBO breath test preparation steps. Stress, irregular sleep, and exercise can all impact gut motility and influence the baseline composition of intestinal bacteria. Discuss any daily routines or potential stressors with your healthcare provider during the preparatory period. They may recommend pausing certain non-critical medications or suggest strategies for limiting lifestyle impacts to ensure consistently accurate breath test outcomes.
Do not make medication adjustments without guidance from a medical provider—safety always takes precedence. Medications that act directly on the gut, such as antacids, laxatives, and antidiarrheal agents, are particularly relevant. The aim is to create an environment within the small intestine that most closely mirrors its natural, unmedicated state. By managing these factors, you maximize the diagnostic value of both hydrogen breath and methane breath assessments.
"Even a single cup of coffee or restricted medication can alter your hydrogen breath test results—follow preparation steps precisely."
Frequently Overlooked Details in SIBO Breath Test Preparation Steps
Meticulous attention to detail sets exceptional SIBO breath test preparation apart from average efforts. Overlooked factors, such as oral hygiene habits or inconsistent timing, can degrade the sensitivity of your results. Brushing your teeth too close to the test or using mouthwash can introduce alcohol or bacteria-disrupting chemicals that impact sample purity. Additionally, varying your water intake or waiting too long between waking and starting your test may disrupt the intestinal bacterial environment the test is intended to measure.
These details—small as they seem—matter significantly. Oral hygiene the night before, exact adherence to fasting, and timing the start of your test collection all play roles in the test’s reliability. By treating every guideline as essential, you reduce the likelihood of ambiguous results and strengthen the accuracy of your small intestinal bacterial overgrowth diagnosis.
Brush teeth the night before, avoiding mouthwash or toothpaste with antibacterial properties close to the test
Begin test immediately upon waking, after the fasting period
Drink only water during the fasting window and avoid excessive amounts near the test time
Have all supplies ready to prevent delays or stress on test day
Document the exact time you begin the test for precise monitoring

People Also Ask: Mastering SIBO Breath Test Preparation Steps
What should you do before a SIBO breath test?
Before a SIBO breath test, follow a strict low-residue, low-fermentation diet for 24 hours, then fast overnight for 12 hours before your appointment. Avoid all non-essential medications, refrain from chewing gum, mints, or smoking, and brush your teeth the night before but not within two hours of the test. It is also crucial to follow any specific instructions provided by your healthcare provider, as proper preparation has a direct impact on the reliability of your test results.
Can I brush my teeth the night before a SIBO test?
Yes, you can and should brush your teeth the night before a SIBO breath test. However, avoid using antibacterial mouthwash or strong toothpaste close to your test time. On the morning of the test, it's best to abstain from brushing until after the test is complete. This ensures no chemical residues alter the composition of your breath sample, maintaining the integrity of your small intestinal bacteria measurement.
What can mess up a SIBO test?
Common pitfalls that can alter the results of a SIBO breath test include eating restricted foods, drinking anything other than water within 12 hours before the test, failing to suspend certain medications (such as antibiotics or probiotics), or inadequate adherence to hygiene requirements. Exercising, chewing gum, or even minor deviations like drinking coffee on test day may also confound accurate detection of small intestinal bacterial overgrowth. Always review and follow your instructions carefully to optimize your test outcomes.
Can you drink water before a SIBO test?
Drinking water is allowed—and even encouraged—during the overnight fasting period leading up to your SIBO breath test. However, avoid excessive intake immediately before or during the test collection process, as this could dilute your breath sample or prompt unintended gut motility. Sticking to moderate sips as needed for comfort generally has no adverse effect on the hydrogen breath test or methane breath test results.
Step-by-Step Guide: Performing the SIBO Breath Test for Small Intestinal Bacterial Overgrowth
The SIBO breath test process is straightforward and yields the best results when you follow your breath test preparation steps precisely. Begin by documenting the time you start the test, ensuring you remain in a calm, undisturbed state. After an initial baseline breath sample is collected, you will drink a sugar solution (usually lactulose or glucose) provided by your medical center or test kit. Over the next two to three hours, you’ll provide additional breath samples at scheduled intervals, carefully sealing each to avoid contamination.
The sequence of collections is designed to track fluctuations in hydrogen and methane gas levels, indicating how the small intestine's bacterial population responds to the introduction of sugars. All test materials, including mouthpieces, vials, and the sugar solution, should be sterilized and handled according to instructions. Consistency and attention to each collection point make a significant difference in diagnosing small intestinal bacterial overgrowth.
Collecting Breath Samples: Ensuring Accuracy in Hydrogen Breath and Methane Breath Tests
When collecting breath samples for your SIBO breath test, it is crucial to follow instructions step by step. Start by exhaling deeply, then breath out completely into the collection device, creating a pure sample for gas measurement. Immediate sealing of the sample ensures that outside air or environmental bacteria do not corrupt the results. Each subsequent sample is collected at pre-set intervals, often every 15 to 20 minutes, depending on the protocol provided by your healthcare provider or medical center.
This sequence is designed to capture real-time changes in gas levels as the sugar solution travels through your gut, highlighting the presence and magnitude of small intestinal bacterial overgrowth. Skipping samples or allowing too much time between collections can skew the data and diminish the reliability of your hydrogen breath test. Remain relaxed, avoid activity during the test, and trust the process for a valid diagnosis.

Timing and Recording Results for the Intestinal Bacterial Overgrowth Diagnosis
Timing your breath sample collections is as critical as the preparation steps themselves. Proper intervals allow your healthcare provider to create a time-resolved map of hydrogen and methane production in your small intestine. Recording the exact start and collection times for each sample ensures any irregularities can be identified and considered in your analysis. Careful documentation enables interpretation of sharp rises or delayed peaks in gas levels—key clues in diagnosing small intestinal bacterial overgrowth versus other GI conditions like lactose intolerance or irritable bowel syndrome.
Use a log or worksheet provided with your SIBO breath test kit to mark times and any notable sensations (like nausea or cramps) you experience during the process. Keeping these records, along with respecting the timing protocols, maximizes the value your healthcare provider can draw from your results and shortens your path to improved gut health.
Demonstration: Best Practices in SIBO Breath Test Sample Collection
FAQs About SIBO Breath Test Preparation Steps, Intestinal Bacteria, and Hydrogen Breath Test
Should I stop probiotics before the test? – Yes, most providers recommend stopping probiotics 1–2 weeks prior unless directed otherwise. Ask your healthcare provider for specific guidance.
Can a low-fiber diet impact my results? – A low-fiber diet minimizes gas malabsorption, making it ideal for a clear baseline during breath tests.
Is timing critical for sample collection? – Absolutely. Every sample must be collected at prescribed intervals to track real-time changes in gas levels accurately.
What if I accidentally eat or drink something prohibited? – Inform your testing provider and consider rescheduling the SIBO breath test to maintain the integrity of your results.
Does travel or stress affect test results? – Travel, disrupted sleep, and stress can all impact gut motility and bacterial composition, so it's best to avoid fluctuations in routine before your test.
Key Takeaways for Optimizing Your SIBO Breath Test Preparation Steps
Strictly follow low-residue dietary guidelines 24 hours before testing.
Fast completely for 12 hours, drinking only water.
Suspend non-essential medications as instructed by your healthcare provider.
Prepare all test materials and begin sample collection immediately upon waking.
Record precise sample times for accurate tracking of hydrogen and methane gas levels.
Communicate with your provider regarding any deviations or concerns before the test.
"Preparation is the cornerstone of accuracy—trust the SIBO breath test preparation steps for confident results."
Conclusion
Follow these SIBO breath test preparation steps meticulously and partner with your provider. With diligence, you’ll achieve valid test results that empower you and your healthcare provider to confidently identify and treat small intestinal bacterial overgrowth.
If you’re committed to improving your digestive health, understanding the role of SIBO breath test preparation is just the beginning. For a more comprehensive approach to wellness, consider how lifestyle changes—such as weight management—can influence not only your gut but also your overall metabolic health. Explore strategies for sustainable weight loss and discover how lowering your cholesterol can have a positive ripple effect on your digestive system and beyond by visiting this in-depth guide to weight loss and cholesterol management. Taking the next step in your health journey can empower you with the knowledge and tools to achieve lasting results.
Sources
NCBI – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6320578/
Mayo Clinic – https://www.mayoclinic.org/tests-procedures/hydrogen-breath-test/about/pac-20384988
Gastroenterology Journal – https://www.gastrojournal.org/article/S0016-5085(19)41282-8/fulltext
To ensure accurate results from your SIBO breath test, it’s crucial to follow specific preparation steps. The article “SIBO Breath Testing Instructions” provides comprehensive guidelines, including dietary restrictions and medication adjustments necessary before the test. (bonheurmd.com)
Additionally, the “Hydrogen Breath Test Preparation for Bacterial Overgrowth” outlines the importance of fasting and other preparatory measures to enhance test accuracy. (health.uconn.edu) By adhering to these detailed instructions, you can significantly improve the reliability of your test results.
 Add Row
Add Row  Add
Add 


Write A Comment