Did you know that as many as 5 million Americans may silently struggle with a stomach condition called gastroparesis—often without even knowing it? This underdiagnosed digestive disorder, gastroparesis, can severely impact your health and daily life, yet many people mistake their gastroparesis symptoms for more common digestive ailments.

In this comprehensive guide, you’ll uncover crucial facts and practical advice about gastroparesis, empowering yourself or loved ones with the knowledge to recognize, treat, and manage this elusive condition.
A Startling Statistic: Why Most People Are Unaware of Gastroparesis
Despite gastroparesis affecting millions, public knowledge remains shockingly low. Many individuals endure symptoms for years, misattributing them to stress, routine indigestion, or other common digestive issues. Medical experts note that the lack of awareness about gastroparesis symptoms significantly contributes to frequent delays in gastroparesis diagnosis. Gastroparesis symptoms—like bloating, feeling full quickly, and stomach pain—are often mistaken for signs of less serious conditions.
This confusion can lead to misdiagnosis, unwarranted treatments, and persistent discomfort. In fact, people with gastroparesis often visit multiple medical professionals before finally receiving a correct diagnosis, affecting their quality of life and heightening frustration.
Many physicians acknowledge that gastroparesis is often overlooked because diagnostic testing for gastric emptying disorders is not routine during initial evaluations. Therefore, people remain unaware that their problem—sluggish stomach emptying—can be caused by a specific condition with real treatment options. It’s crucial to bring awareness to the statistics and realities of living with this disorder and encourage early evaluation when persistent signs appear.
Unveiling the Prevalence of Gastroparesis in the United States
Although the figures vary, studies estimate that up to 5 million Americans may experience gastroparesis during their lifetime. Unfortunately, many cases remain undiagnosed due to vague symptoms and lack of screening. The majority of cases affect women, with idiopathic gastroparesis—where no clear cause is found—being the most common. Experts believe increased awareness among both patients and healthcare professionals is key to reducing delayed diagnoses and improving outcomes.
"This disease is a physical illness that can become a psychiatric illness very quickly because it's very isolating. These patients are socially isolated. They don't want to go out to eat because they get sick when they eat." (Source: Cleveland Clinic)
Understanding Gastroparesis: Definition, Causes, and Mechanisms

What is Gastroparesis and How Does it Disrupt Gastric Emptying?
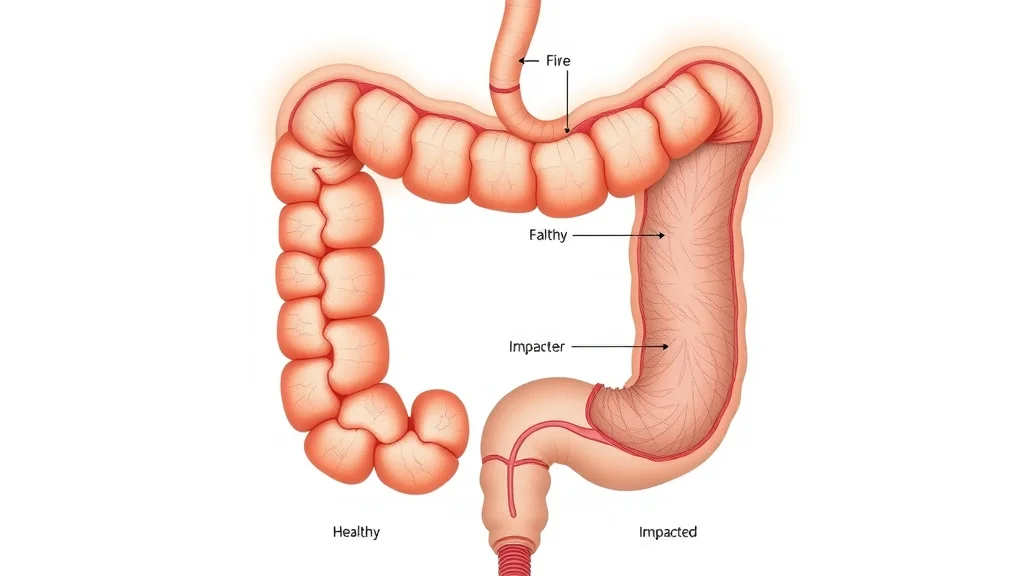
Gastroparesis is a chronic digestive disorder characterized by delayed gastric emptying, a condition where the stomach empties its contents into the small intestine much slower than normal—not due to a blockage, but because of impaired muscle or nerve function, including potential vagus nerve dysfunction. This delayed gastric emptying leads to symptoms like nausea, vomiting, feeling full too soon when starting a meal, and often unexplained weight loss. Food sits in the stomach longer than it should, sometimes forming a mass called a bezoar, which worsens symptoms and can obstruct food passage. Over time, people with gastroparesis may develop nutritional deficiencies and poor blood sugar control, especially if they have diabetes.
The severity and frequency of symptoms can vary widely. Some individuals may experience mild discomfort, while others struggle with recurrent nausea and vomiting. Diagnosing gastroparesis is crucial because gastroparesis symptoms often overlap with those of functional dyspepsia or irritable bowel syndrome (IBS), potentially causing delays in effective gastroparesis treatment. Understanding the underlying disruption in gastric emptying is essential for recognizing and managing this condition effectively.
Since gastroparesis can sometimes lead to unintended weight changes, it's important to understand how shifts in body weight might impact other aspects of health. For those curious about the connection between weight loss and related symptoms, exploring the relationship between weight loss and hair health can provide additional insight into the broader effects of digestive disorders.
The Physiology of Gastric Emptying and Gastroparesis
The stomach plays a critical role in digestion by acting as a reservoir for food and controlling gastric emptying through the slow release of its contents into the small intestine. This process, known as gastric emptying, relies on coordinated contractions of stomach muscles and signals from the vagus nerve, which help churn and propel food through the digestive tract. In gastroparesis, these contractions are weak or disorganized, leading to abnormally slow stomach emptying without an identifiable obstruction.
When this natural movement falters, nutrients and calories are not absorbed as efficiently, which can result in malnutrition and unintended weight loss. The delayed movement can also disrupt blood sugar levels, particularly in people with diabetes, making their condition harder to manage. When food lingers, it increases the risk of bacterial overgrowth and creates an environment ripe for the development of a mass called a bezoar. For patients, this means symptoms don't just disrupt comfort—they disrupt daily life and overall health.
Primary Causes and Risk Factors Behind Gastroparesis
Gastroparesis can result from several underlying factors, with diabetes being the most frequently identified medical condition linked to the development of gastroparesis. High blood sugar levels over time can damage nerves that control stomach muscles, leading to gastroparesis as a common side effect. Besides diabetes, other risk factors include certain medications (such as narcotics and some antidepressants), past stomach surgeries that disrupt nerves or muscles, and viral infections that impact the digestive tract.
In many cases, however, the cause remains idiopathic—meaning no clear reason is found. This makes diagnosing gastroparesis particularly challenging and can leave patients searching for answers and relief. Awareness about risk factors, even for those without diabetes, is essential to identifying symptoms early and reducing the risk of complications.
Diabetes (poorly controlled blood sugar)
Certain medications (narcotics, some antidepressants)
Previous abdominal or stomach surgeries
History of viral infection
Idiopathic causes (unknown origin)
Gastroparesis Symptoms: Recognizing the Early Warning Signs
Common Symptoms of Gastroparesis
Early recognition of symptoms of gastroparesis can significantly improve the effectiveness of gastroparesis treatment and overall management. Most people with gastroparesis report feeling full after eating only a small amount, even when hungry at the start of a meal. Nausea and vomiting, particularly of undigested food hours after eating, are also classic clues. Persistent abdominal pain, bloating, and unintentional weight loss are additional warning signs.
"The outcomes of treating gastroparesis are not always perfect, and not the same for every individual. That said, it is a condition which can be treatable. I give LaKisha a great deal of credit for her commitment and resilience. She's as much her own doctor as I am." (Source: Dr. Brooks Cash, Chief of the Division of Gastroenterology, Hepatology, and Nutrition at UTHealth Houston
Some patients may have intermittent symptoms, while others experience chronic discomfort and noticeable changes in eating habits. This unpredictability often leads to repeated doctor visits and confusion about the source of the distress. If you or someone you know frequently struggles with these issues, it's important to consider the possibility of gastroparesis and discuss testing or referrals to a gastroenterologist.
Nausea
Vomiting (especially undigested food)
Abdominal pain and bloating
Feeling full soon after eating (early satiety)
Appetite loss and weight loss
How Symptoms of Gastroparesis Differ from Other Digestive Disorders
It is not uncommon for people to confuse gastroparesis symptoms with those of other gastrointestinal conditions, like IBS or GERD. However, symptoms that stand out for gastroparesis include persistent delayed gastric emptying and vomiting of undigested—or partly digested—food several hours after meals. Unlike GERD (acid reflux) or IBS, which are driven by different mechanisms, the hallmark of gastroparesis is the stomach’s inability to empty at a normal rate.
Additionally, people with gastroparesis often report poor response to typical GERD or IBS medications, which can be a clue for healthcare providers. Recognizing these nuanced differences improves diagnostic accuracy and guides doctors toward ordering appropriate tests, rather than solely relying on medication trials that may not address the underlying problem.
Comparison: Gastroparesis Symptoms vs IBS and GERD Symptoms
Symptom |
Gastroparesis |
IBS |
GERD |
|---|---|---|---|
Nausea |
Frequent, after eating |
Occasional |
Occasional |
Vomiting |
Common (undigested food hours after eating) |
Rare |
Rare (usually with severe reflux) |
Bloating |
Common and persistent |
Common |
Occasional |
Feeling full early |
Very common |
Sometimes |
Sometimes |
Abdominal pain |
Frequent |
Frequent |
Occasional, burning type |
Acid reflux/heartburn |
Sometimes (related to stasis) |
Rare |
Common |
Weight loss |
Common, unexplained |
Rare |
Rare |

Diagnosis: How is Gastroparesis Detected and Differentiated?
Gastroparesis Diagnostic Tests: From Gastric Emptying Studies to Imaging
Diagnosing gastroparesis involves a thorough medical history, symptom assessment, and specialized diagnostic tests, including gastric emptying studies, to confirm delayed gastric emptying. Standard blood work may rule out other causes, but does not confirm gastroparesis itself. The cornerstone diagnostic test for gastroparesis is a gastric emptying study (gastric emptying scintigraphy), which involves eating a small meal tagged with a harmless radioactive marker. Images are taken over several hours to determine how quickly food passes from the stomach. A delayed rate confirms gastroparesis.
Newer technologies, such as the SmartPill (a wireless motility capsule), can track the passage of food and measure pH, temperature, and pressure throughout the digestive tract. Imaging studies, like abdominal ultrasound and upper endoscopy, help exclude structural causes of obstruction, while simultaneously evaluating for other gastrointestinal conditions. It’s important to perform these tests under the guidance of a knowledgeable gastroenterologist, as accurate diagnosis shapes the entire management strategy.
Gastric Emptying Scintigraphy
SmartPill (wireless motility capsule)
Upper Endoscopy
Abdominal Ultrasound
The Role of Medical History and Symptom Tracking
The journey to a gastroparesis diagnosis typically starts with a thorough review of the patient’s medical history and an in-depth discussion of symptoms. Doctors will ask about timing and duration of gastroparesis symptoms, their relation to meals, prior medical or surgical history, and any long-term medications that could affect digestive motility. Careful physical exam and documentation of changing symptoms over time can uncover patterns suggestive of delayed gastric emptying.
Symptom tracking—using diaries or smartphone apps—can help patients identify triggers and help doctors distinguish gastroparesis from functional GI disorders. This collaborative approach between patient and practitioner ensures early clues are not missed and paves the way for more effective diagnosis and individualized treatment strategies.
Comprehensive Gastroparesis Treatment: Managing and Relieving Symptoms
Medical and Dietary Gastroparesis Treatment Approaches
Gastroparesis treatment requires a personalized approach, often combining medications, dietary modifications, and lifestyle adjustments to effectively manage gastroparesis symptoms. Top goals of gastroparesis treatment include relieving gastroparesis symptoms, maintaining nutrition, and improving quality of life. Medical treatment often involves prokinetic medications that stimulate stomach muscle contractions, antiemetic drugs for nausea, and addressing underlying risk factors, like high blood sugar in diabetics. In severe cases, placement of a feeding tube may be necessary if oral intake cannot sustain nutritional needs.
Diet is a cornerstone of management. Patients are typically advised to eat smaller, more frequent meals and to avoid high-fat, high-fiber foods that slow stomach emptying further. Some may benefit from pureed or liquid diets. In rare situations where symptoms are severe and unresponsive to conservative measures, gastric electrical stimulation (a device that delivers mild pulses to stomach muscles) or even surgery may be considered. Each treatment plan is tailored to the individual's unique symptoms and overall health.
Medications (prokinetics, antiemetics)
Dietary modifications
Electrical stimulation of the stomach
Surgical interventions (where indicated)

Daily Life with Gastroparesis: Nutrition, Meal Planning, and Lifestyle Strategies
Living with gastroparesis involves continuous adjustments to diet and daily habits to effectively manage gastroparesis symptoms and improve quality of life. The best approach is to focus on easily digestible foods—such as cooked vegetables, low-fat proteins, and blended meals—that pass through the stomach with minimal effort. Avoiding raw vegetables, tough meats, and high-fiber foods can reduce symptom flare-ups. Staying hydrated and supplementing with nutritional shakes may be advised, especially during episodes of severe symptoms.
Many people find that eating smaller meals spaced throughout the day, chewing food thoroughly, and resting upright after eating are helpful lifestyle modifications. Nutrition counseling with a registered dietitian can customize meal plans, monitor weight loss risk, and identify gaps in nutrition. Support groups and mental health counseling can also help patients and families cope with the emotional stress of managing a chronic digestive disorder.
Sample Meal Plans and Dietary Suggestions for Gastroparesis
Meal |
Examples |
|---|---|
Breakfast |
Oatmeal with banana slices, scrambled eggs, apple sauce |
Lunch |
Chicken broth with soft noodles, poached fish, mashed carrots |
Snack |
Low-fat yogurt, fruit smoothie (no skins or seeds) |
Dinner |
Baked sweet potato (no skin), lean ground turkey, green beans (well-cooked) |
Beverages |
Water, diluted juice, herbal tea, meal replacement shakes |

Living with Gastroparesis: Real Patient Stories and Insights
Personal experiences highlight the day-to-day challenges and triumphs of those living with gastroparesis. From navigating social meals and learning to advocate for their health, patients describe how they’ve adapted to new routines and dietary changes. Many report relief at finally understanding the cause of their distress and finding treatment plans that work for them.
"I struggled for years before finding a diagnosis for my gastroparesis. It changed my approach to eating and living." – Gastroparesis Patient
Support from healthcare professionals, friends, and online communities can make a significant difference. Sharing stories and advice helps others with unknown digestive symptoms seek evaluation, find relief, and realize they’re not alone on their journey.
People Also Ask About Gastroparesis
What does mild gastroparesis feel like?
Mild gastroparesis often presents with subtle symptoms, such as feeling full quickly after starting a meal, mild nausea, or occasional bloating. Some people notice a sense of delayed digestion or slight abdominal discomfort after eating, but these symptoms may come and go, making diagnosis tricky. Early recognition is key to preventing progression and ensuring proper management.
Does gastroparesis go away on its own?
For most people, gastroparesis does not resolve spontaneously. While mild cases linked to temporary factors—like a viral infection—may improve, chronic cases require ongoing management through medications, dietary changes, and careful symptom monitoring. Early intervention and addressing underlying causes can prevent complications and improve long-term outcomes.
What can you not eat with gastroparesis?
People with gastroparesis are advised to avoid foods that are difficult to digest or slow stomach emptying. These include high-fat foods, raw vegetables, tough cuts of meat, beans, fibrous fruits (like oranges or pineapple), seeds, nuts, and whole grains with intact fiber. Sticking to soft, well-cooked, or pureed foods typically helps minimize risks of symptom flare-ups.
What calms gastroparesis?
Managing gastroparesis symptoms often requires a combination of dietary changes, symptom-relieving medications, and lifestyle adjustments. Eating smaller meals, staying hydrated, resting upright after eating, and working with a dietitian to develop a personalized plan can all help calm gastroparesis. In some cases, medications or stress management techniques can provide additional relief.

FAQs: Essential Answers About Gastroparesis
Is gastroparesis curable?
Gastroparesis is typically a long-term condition, but many people experience significant improvement through individualized treatment. While a permanent cure is rare, symptoms can often be controlled, and patients can maintain an excellent quality of life with careful management and support.
What is the life expectancy with gastroparesis?
Most people with gastroparesis have a normal life expectancy, especially with good symptom management and attention to nutrition. Complications, like malnutrition or repeated severe infections, can rarely impact longevity, making regular follow-up and prompt treatment vital.
Can children develop gastroparesis?
Yes, children can develop gastroparesis. In pediatric cases, causes may include viral infections, diabetes, or be idiopathic. Because symptoms can mimic other childhood digestive problems, a specialist’s evaluation is important to ensure the right diagnosis and a balanced treatment plan.
Are there any new treatments for gastroparesis?
Advances in gastroparesis treatment include new medications that stimulate gastric motility, endoscopic techniques, and improved devices for gastric electrical stimulation. Research continues to explore more effective therapies with fewer side effects, giving hope for better symptom control in the future.
How is gastroparesis different from functional dyspepsia?
While both conditions may cause early satiety, nausea, and bloating, gastroparesis is characterized by objectively measured delayed gastric emptying. Functional dyspepsia, on the other hand, appears normal on diagnostic tests, making the assessment of symptoms and testing critical for accurate diagnosis.
Key Takeaways: Understanding and Managing Gastroparesis
Gastroparesis is a common yet often underdiagnosed digestive condition.
Symptoms are vague and easily mistaken for other gastrointestinal disorders.
Prompt diagnosis and tailored treatment are crucial for relief and prevention of complications.
Dietary and lifestyle adjustments are key to living well with gastroparesis.
Conclusion: Empowering Yourself with Knowledge About Gastroparesis
Awareness is the best defense against hidden health risks like gastroparesis. Know the symptoms, seek specialist help early, and take charge of your digestive health for a brighter, healthier future.
If you’re interested in taking your digestive wellness journey even further, consider exploring the broader landscape of nutrition and foods that support gut health. The Nutrition & Foods resource hub offers a wealth of expert-backed articles, meal ideas, and advanced strategies for optimizing your diet.
Whether you’re managing gastroparesis or simply aiming to enhance your overall well-being, these insights can help you make informed choices and discover new ways to nourish your body. Dive deeper to unlock practical tips and inspiration for a healthier, more vibrant lifestyle.
Sources
Gastroparesis is a condition that affects the stomach’s ability to empty its contents properly, leading to symptoms such as nausea, vomiting, and abdominal pain. For a comprehensive understanding of this condition, the Mayo Clinic’s article, “Gastroparesis - Symptoms and causes,” provides detailed information on its symptoms, causes, and potential complications.
Additionally, the National Institute of Diabetes and Digestive and Kidney Diseases offers an in-depth resource titled “Gastroparesis,” which covers aspects such as diagnosis, treatment options, and dietary recommendations. If you’re seeking to deepen your knowledge about gastroparesis, these resources offer valuable insights and guidance.
 Add Row
Add Row  Add
Add 


Write A Comment