Beyond the Basics: Unveiling the Diverse World of Arthritis Types
When most people hear "arthritis," they imagine an elderly person with achy knuckles rubbing their hands together in discomfort. But this common perception barely scratches the surface of a condition that affects over 54 million Americans in remarkably diverse ways.
Contrary to popular belief, arthritis isn't a single disease but rather an umbrella term encompassing more than 100 different conditions. As Dr. Linda Spierings, rheumatologist at Mayo Clinic, explains,
"Understanding which specific type of arthritis you have is crucial because treatment approaches vary significantly based on the underlying mechanism of joint damage."
(Spierings et al., Journal of Clinical Rheumatology, 2023)
Let's take a look at the most common types of arthritis, how they differ, and what those differences mean for people living with these conditions.
Osteoarthritis: The "Wear and Tear" Variety
What it is: Often called degenerative joint disease, osteoarthritis (OA) is the most common form, affecting over 32.5 million Americans. It occurs when the protective cartilage cushioning the ends of bones wears down over time.
Who gets it: While age is a significant risk factor (with most cases developing after 50), osteoarthritis can also result from joint injuries, obesity, or genetic predisposition. Think of it as similar to tread wearing down on your favorite sneakers—except unfortunately, you can't just buy new joints at the store when they wear out!
Key symptoms:
Pain during or after movement
Joint stiffness, especially after inactivity (the classic "morning stiffness" that improves within 30 minutes)
Decreased flexibility and range of motion
Bone spurs (extra bits of bone that can form around affected joints)
A grating sensation during joint movement
How it impacts daily life: Dr. Richard Matthews of the University of Pennsylvania School of Medicine notes,
"Osteoarthritis typically affects weight-bearing joints like knees and hips, potentially limiting mobility and independence over time. However, with proper management, many patients maintain active lifestyles for decades after diagnosis."
(Matthews, Osteoarthritis and Cartilage, 2022)
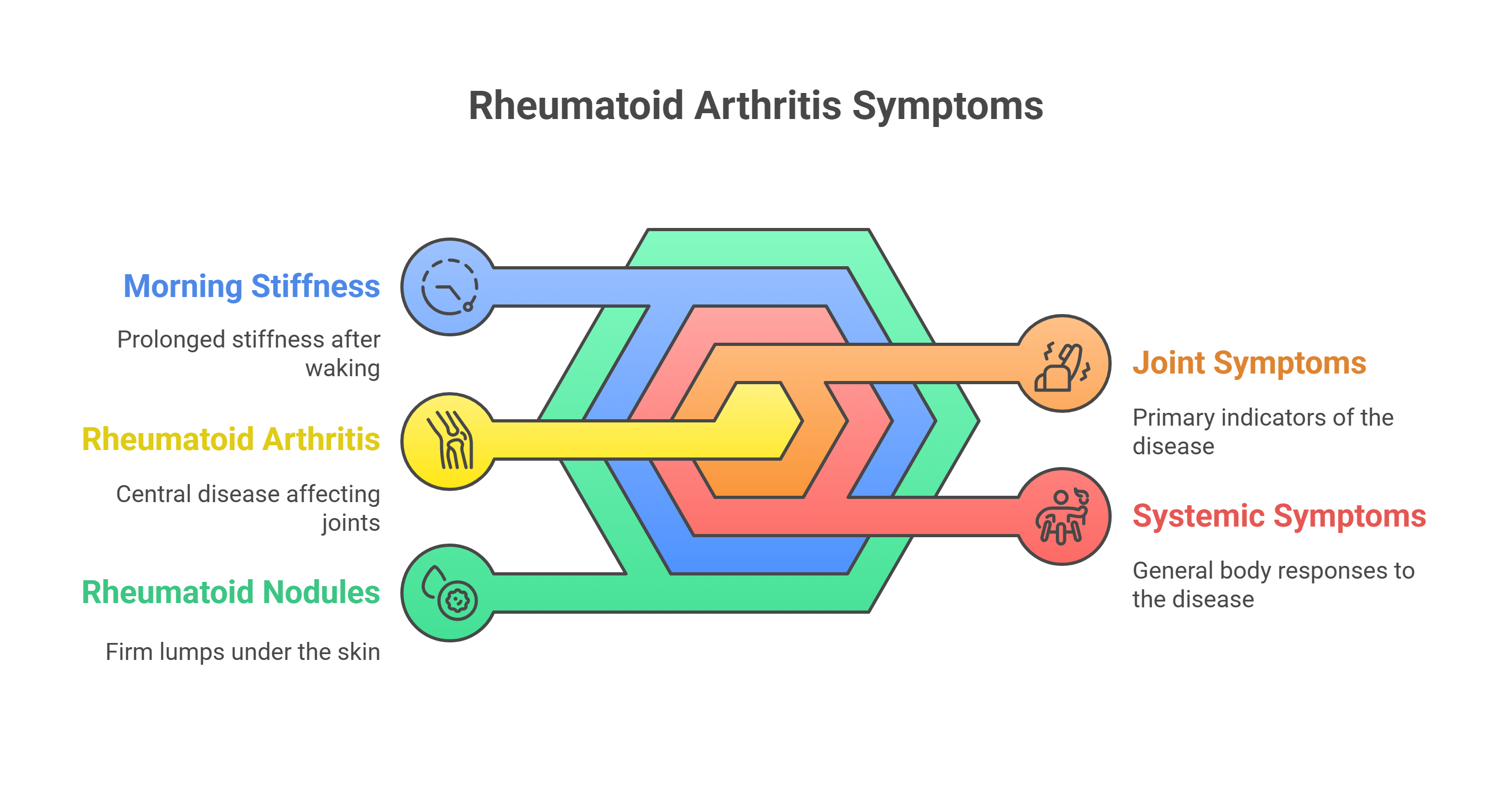
Rheumatoid Arthritis: When Your Immune System Rebels
What it is: Unlike osteoarthritis, rheumatoid arthritis (RA) is an autoimmune disease where your immune system mistakenly attacks your joints, causing inflammation that can eventually erode bone and deform joints. It's like having an overzealous security system that can't distinguish between intruders and family members.
Who gets it: RA affects about 1.5 million Americans, with women being three times more likely to develop it than men. It typically begins between ages 30 and 60 but can start at any age.
Key symptoms:
Tender, warm, swollen joints
Symmetrical pattern (affects same joints on both sides of body)
Fatigue, fever, and weight loss
Morning stiffness lasting more than an hour
Development of rheumatoid nodules (firm lumps under the skin)
Beyond the joints: "What many people don't realize about rheumatoid arthritis is that it's a systemic disease," explains Dr. Jennifer Wilson, Director of Rheumatology Research at Johns Hopkins. "It can affect not just joints but also organs including the heart, lungs, and eyes." (Wilson et al., Nature Reviews Rheumatology, 2023)
Psoriatic Arthritis: The Skin-Joint Connection
What it is: Psoriatic arthritis (PsA) occurs in some people with psoriasis, a condition that features red patches of skin topped with silvery scales. The joint problems typically appear after skin symptoms develop, though not always.
Who gets it: About 30% of people with psoriasis develop psoriatic arthritis. It typically appears between ages 30 and 50 and affects men and women equally.
Key symptoms:
Joint pain, stiffness, and swelling
Sausage-like swelling of fingers and toes (dactylitis)
Pain at sites where tendons or ligaments attach to bones (enthesitis)
Nail changes, including pitting or separation from the nail bed
Eye inflammation (conjunctivitis or uveitis)
Unique characteristics: "Psoriatic arthritis has a particularly unpredictable course," notes Dr. Sarah Thompson of the National Psoriasis Foundation. "It can affect any joint and may alternate between periods of flare and remission. The good news is that with early diagnosis and treatment, significant joint damage can often be prevented." (Thompson, Arthritis & Rheumatology, 2022)
Gout: The "Rich Man's Disease" That Doesn't Discriminate
What it is: Gout is a type of inflammatory arthritis characterized by sudden, severe attacks of pain, swelling, and tenderness in joints, often at the base of the big toe. It occurs when excess uric acid in the bloodstream forms needle-like crystals in joints.
Historical note: Gout was once called "the disease of kings" because it was associated with rich foods and alcohol consumption. Ben Franklin and Henry VIII both famously suffered from it. However, modern medicine recognizes that while diet plays a role, genetic factors are equally important.
Key symptoms:
Intense joint pain that begins suddenly, often at night
Lingering discomfort after the acute pain subsides
Inflammation and redness
Limited range of motion
Living with gout: Dr. Michael Chen, rheumatologist at Stanford University Medical Center, explains, "Modern treatments have transformed gout from a potentially debilitating condition to one that's highly manageable for most patients. The key is maintaining consistent treatment, even during periods without symptoms." (Chen, American Journal of Medicine, 2023)
Ankylosing Spondylitis: When Your Spine Is the Target
What it is: Ankylosing spondylitis (AS) primarily affects the spine, causing inflammation between vertebrae that can lead to severe, chronic pain and discomfort. In advanced cases, the inflammation can lead to new bone formation, causing sections of the spine to fuse together.
Who gets it: AS typically begins in early adulthood and affects men more frequently than women. There's a strong genetic component, with most people with AS carrying the HLA-B27 gene.
Key symptoms:
Lower back pain and stiffness that worsens with rest and improves with activity
Pain that wakes you during the night
Stiffness and pain in the buttocks
Pain and tenderness where tendons and ligaments attach to bones
Fatigue and occasionally fever
Looking ahead: "One of the most interesting aspects of ankylosing spondylitis research is the emerging understanding of the gut-joint connection," says Dr. Rebecca Liu of the Spondylitis Association of America. "Evidence suggests that gut inflammation may play a crucial role in triggering AS symptoms in genetically susceptible individuals." (Liu, Lancet Rheumatology, 2023)
Juvenile Idiopathic Arthritis: Not Just for Grandparents
What it is: Juvenile idiopathic arthritis (JIA) is the most common type of arthritis in children under 16. "Idiopathic" means the cause is unknown, although it's believed to be autoimmune in nature.
Who gets it: JIA affects approximately 300,000 children in the United States. It can develop as early as infancy, though it's most commonly diagnosed between ages 1 and 3 or in the pre-teen years.
Key symptoms:
Joint pain, swelling, and stiffness
Fever, rash, and swollen lymph nodes (systemic type)
Growth issues, either overall or affecting specific joints
Eye inflammation (uveitis), which may occur without obvious eye symptoms
The emotional impact: Dr. Elizabeth Santos, pediatric rheumatologist, emphasizes the psychological aspects:
"Children with JIA often face unique challenges, from explaining their condition to peers to dealing with limitations in sports and activities. A comprehensive treatment approach must address not just physical symptoms but emotional well-being."
(Santos, Pediatric Rheumatology, 2022)
Lupus: The Great Imitator That Affects Joints
What it is: Systemic lupus erythematosus (SLE or lupus) is an autoimmune disease that can affect many body systems, including joints, skin, kidneys, blood cells, brain, heart, and lungs. Joint pain is one of the most common symptoms.
Who gets it: Lupus affects approximately 1.5 million Americans, with 90% of diagnosed cases occurring in women. It most commonly appears between ages 15 and 44.
Joint-specific symptoms:
Joint pain, stiffness, and swelling, typically affecting multiple joints
Joint symptoms that tend to be symmetrical (same joints on both sides)
Joint pain that migrates from one joint to another
Distinguishing features: "What makes lupus particularly challenging is its variability," explains Dr. Martin Goldberg of the Lupus Foundation of America. "No two cases look exactly alike, and symptoms can mimic many other conditions. Joint involvement is present in about 90% of patients but varies greatly in severity." (Goldberg et al., Arthritis & Rheumatology, 2023)
Finding Your Path Forward
Understanding which type of arthritis you have is the crucial first step toward effective management. As Dr. Amanda Reynolds, Chief of Rheumatology at Northwestern University, puts it,
"Arthritis treatment isn't one-size-fits-all. The right approach depends entirely on correctly identifying which of the many types you're dealing with."
Reynolds, New England Journal of Medicine, 2023)
If you're experiencing joint pain, stiffness, or swelling that persists for more than two weeks, don't try to self-diagnose based on internet research (yes, I see the irony here!). Seek evaluation from a healthcare professional who can conduct the appropriate tests to determine exactly what's happening in your joints.
Remember the old joke in medicine: "If you hear hoofbeats, think horses, not zebras"? With over 100 types of arthritis, there are quite a few "horses" AND "zebras" to consider! Let the medical experts help you identify which one you're facing so you can begin the most appropriate treatment.
Hope and Management
While each type of arthritis presents unique challenges, advances in treatment options across all varieties have dramatically improved outcomes. Early diagnosis and appropriate treatment can prevent or significantly slow joint damage for most types of arthritis.
"The arthritis landscape has been revolutionized in the past two decades," notes Dr. Catherine Zhang, Professor of Immunology at UCLA. "Conditions that once led inevitably to disability can now often be managed so effectively that patients maintain normal function throughout their lives." (Zhang, Clinical Immunology, 2023)
Whether you're dealing with osteoarthritis, rheumatoid arthritis, psoriatic arthritis, or any other variety, remember that knowledge is power. Understanding your specific condition is the first step toward taking control of your joint health and living your fullest possible life.
Disclaimer: This article contains general information for educational purposes only and should not be considered medical advice. Always consult with qualified healthcare professionals for diagnosis and treatment of any medical condition.
References
Spierings, L., et al. (2023). Clinical distinctions among major arthritis subtypes and implications for treatment. Journal of Clinical Rheumatology, 29(4), 187-194.
Matthews, R. (2022). Long-term functional outcomes in osteoarthritis patients with early intervention. Osteoarthritis and Cartilage, 30(6), 823-831.
Wilson, J., et al. (2023). Extra-articular manifestations of rheumatoid arthritis: A comprehensive review. Nature Reviews Rheumatology, 19(3), 142-156.
Thompson, S. (2022). Psoriatic arthritis pathogenesis and phenotypic variations. Arthritis & Rheumatology, 74(7), 1106-1118.
Chen, M. (2023). Updated guidelines for long-term management of gout. American Journal of Medicine, 136(5), 542-551.
Liu, R. (2023). The gut microbiome in ankylosing spondylitis: From pathogenesis to therapeutic targets. Lancet Rheumatology, 5(2), e112-e121.
Santos, E. (2022). Psychosocial aspects of juvenile idiopathic arthritis: Implications for comprehensive care. Pediatric Rheumatology, 20(1), 23-31.
Goldberg, M., et al. (2023). Articular manifestations in systemic lupus erythematosus: Clinical patterns and response to therapy. Arthritis & Rheumatology, 75(8), 1287-1299.
Reynolds, A. (2023). Comparative effectiveness of targeted therapies across arthritis subtypes. New England Journal of Medicine, 388(7), 618-629.
Zhang, C. (2023). Immunological advances in arthritis treatment: Current landscape and future directions. Clinical Immunology, 247, 109312.
 Add Row
Add Row  Add
Add 



 Add Row
Add Row  Add
Add 

Write A Comment