
What You Need To Know About Endometriosis And Its Symptoms
Endometriosis, a perplexing and often debilitating condition, manifests when tissue akin to the uterine lining, the endometrium, ventures beyond its typical confines within the uterus. This errant tissue can establish itself on various pelvic organs, including the ovaries and fallopian tubes, and even extend to the outer uterine surface. In less frequent scenarios, it has been observed in more distant parts of the body.
Dr. Iris Kerner, a reproductive endocrinologist, highlights the fundamental mechanism of this misplaced tissue, stating,
"The crucial aspect to understand is that these endometrial-like implants, wherever they reside, retain their responsiveness to the cyclical hormonal fluctuations of menstruation. They thicken, break down, and bleed in synchrony with the uterine lining."
This monthly activity outside the uterus, however, lacks a natural exit route, culminating in inflammation, the formation of scar tissue (adhesions that can bind organs), and the potential development of fluid-filled cysts known as endometriomas, particularly affecting the ovaries.
The symptomatic landscape of endometriosis is remarkably diverse. As Dr. Neil Johnson, a leading expert in the field, emphasizes in a 2017 review published in the New England Journal of Medicine,
"The correlation between the extent of endometriotic lesions and the severity of symptoms is often surprisingly weak. Some individuals with minimal disease experience excruciating pain, while others with extensive involvement report only mild discomfort."
This variability underscores the complex and individualized nature of the condition. Common manifestations include intensely painful periods (dysmenorrhea) that can disrupt daily life, chronic pelvic pain independent of menstruation, discomfort during or after sexual intercourse (dyspareunia), pain associated with bowel movements or urination (often exacerbated during menses), heavy or irregular menstrual bleeding, fatigue, and challenges with fertility. Digestive disturbances, such as bloating and altered bowel habits, can also be prominent features.

The diagnostic journey for endometriosis can be protracted. While clinical suspicion may arise from a thorough medical history and pelvic examination, the gold standard for definitive diagnosis remains laparoscopy. Dr. Sarah Berga, a professor of obstetrics and gynecology, explains this procedure as,
"A minimally invasive surgical approach allowing direct visualization of the pelvic cavity. Through small incisions, a camera is introduced, enabling the surgeon to identify and potentially excise or biopsy suspicious lesions for histological confirmation."
While imaging techniques like pelvic ultrasound and MRI can offer supportive evidence, particularly in identifying endometriomas or deep infiltrating endometriosis, they cannot definitively diagnose the disease.
The precise origins of endometriosis remain an area of active research, with several compelling theories proposed. Retrograde menstruation, the backward flow of menstrual blood through the fallopian tubes, is a widely considered mechanism, suggesting that these displaced endometrial cells may then implant and proliferate. Another hypothesis involves the transformation of peritoneal cells, where hormonal or immunological signals may induce cells lining the abdominal cavity to adopt endometrial-like characteristics.

Embryonic cell metaplasia proposes that remnants of embryonic tissue may differentiate into endometrial-like tissue during puberty. Surgical procedures can also inadvertently lead to the implantation of endometrial cells at scar sites. Furthermore, a familial predisposition suggests a genetic component, and immune system dysfunction may impair the body's ability to clear misplaced endometrial tissue.
Management strategies for endometriosis are tailored to the individual's specific needs and goals, as there is currently no definitive cure. Treatment aims to alleviate symptoms, slow disease progression, and address fertility concerns. Pharmacological interventions include pain relievers and hormonal therapies, such as oral contraceptives, progestins, and GnRH agonists, which can suppress endometrial tissue growth and reduce pain.
Surgical options range from laparoscopic excision or ablation of endometriotic lesions and adhesions to hysterectomy, often with oophorectomy, reserved for severe, refractory cases in individuals who have completed childbearing. For those experiencing infertility associated with endometriosis, assisted reproductive technologies like IVF may be recommended.
Ultimately, a collaborative approach between the individual and their healthcare provider is crucial for effective management of this intricate condition, emphasizing the importance of personalized care and ongoing support.
Endometriosis FAQ:
This FAQ provides insights into living with endometriosis, drawing upon the expertise of medical professionals.
Q: Can you live normally with endometriosis?
A: Living "normally" with endometriosis is a very personal experience and depends significantly on the severity of symptoms and the effectiveness of management strategies. Dr. Iris Kerner, a reproductive endocrinologist, notes,
"While endometriosis can profoundly impact daily life due to pain, fatigue, and other symptoms, many individuals find ways to manage their condition effectively through a combination of medical treatments, lifestyle adjustments, and support systems. It's about finding a new 'normal' that accommodates the challenges while maximizing quality of life."
This often involves proactive management and a strong partnership with healthcare providers.
Q: Can endometriosis go away?
A: Currently, there is no known cure for endometriosis in the conventional sense. While symptoms can be managed and the progression of the disease potentially slowed, it doesn't typically disappear on its own. Dr. Neil Johnson, in his extensive review, states,
"Spontaneous regression of endometriosis is not well-documented in the medical literature. While hormonal fluctuations, particularly after menopause, can lead to a decrease in activity of the lesions, the underlying condition generally persists."
Certain treatments, such as hysterectomy with the removal of ovaries, can provide a long-term solution by eliminating the hormonal drivers of the disease, but this is a significant surgical intervention.
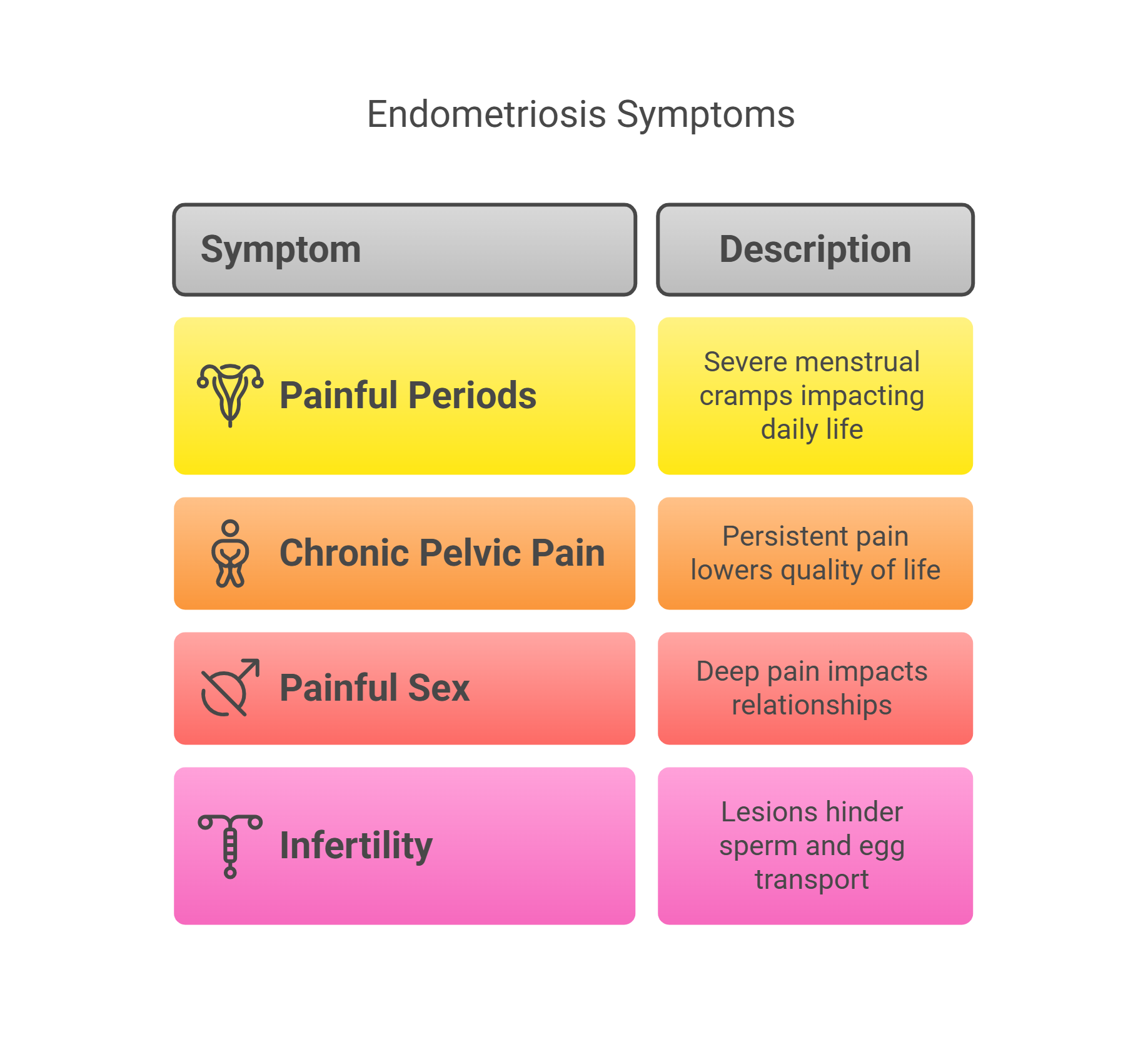
Q: What are 4 symptoms of endometriosis?
A: Endometriosis presents with a diverse range of symptoms, but some of the most commonly reported include:
Painful periods (dysmenorrhea): Dr. Sarah Berga, a professor of obstetrics and gynecology, emphasizes that this pain is often "more severe than typical menstrual cramps and can be debilitating, impacting work, school, and social activities."
Chronic pelvic pain: This pain can be present even outside of menstruation. Dr. Kerner explains that this "persistent ache or sharp pain in the pelvic region can significantly lower a person's baseline quality of life."
Pain during or after sex (dyspareunia): This deep pain with intercourse is a frequent complaint.According to Dr. Johnson, "Dyspareunia can have a significant emotional and relational impact, often being underreported."
Infertility: Endometriosis can interfere with natural conception. Dr. Berga notes that "the presence of endometrial lesions and adhesions can distort pelvic anatomy and hinder the transport of sperm and egg."
Q: What does living with endometriosis look like?
A: Living with endometriosis is a multifaceted experience. It often involves navigating chronic pain, which can fluctuate in intensity and impact daily functioning. Dr. Kerner points out that
"individuals may experience periods of relative calm interspersed with flares of intense pain, requiring careful planning of activities and reliance on pain management strategies."
Fatigue is another common and often underestimated symptom that can significantly affect energy levels and the ability to perform daily tasks. Furthermore, the emotional toll of living with a chronic and often invisible illness can be substantial, potentially leading to anxiety and depression. As Dr. Johnson highlights,
"The uncertainty of symptom onset and the potential impact on fertility and relationships contribute to the psychological burden of endometriosis."
Access to knowledgeable healthcare professionals and strong support networks are crucial for navigating the complexities of this condition.
Q: What is the life expectancy of a person with endometriosis?
A: Endometriosis is not considered a life-threatening condition and does not inherently reduce life expectancy. Dr. Sarah Berga clarifies,
"Endometriosis primarily affects quality of life due to its symptoms. It is not associated with an increased risk of mortality in the way that conditions like cancer or heart disease are."
While the chronic pain and other symptoms can be debilitating, they do not directly impact lifespan. Management focuses on alleviating these symptoms and improving overall well-being.
Q: Can endometriosis cause weight gain?
A: The direct link between endometriosis and weight gain is not definitively established, and it's an area where more research is needed.However, some indirect factors associated with endometriosis and its treatment could potentially contribute to weight fluctuations. Dr. Iris Kerner explains,
"Hormonal therapies, which are commonly used to manage endometriosis symptoms, can sometimes have weight gain as a side effect in some individuals. Additionally, reduced physical activity due to chronic pain and fatigue might indirectly contribute to weight changes."
It's important for individuals with endometriosis to discuss any concerns about weight changes with their healthcare provider to determine the underlying cause and appropriate management strategies.
 Add Row
Add Row  Add
Add 




 Add Row
Add Row  Add
Add 

Write A Comment