Did you know a coronary artery calcium score can predict your risk of heart disease years before symptoms appear? Understanding this simple test could be key to preventing a heart attack and saving your life. Let’s explore how this score offers crucial insights into your heart health.

Why Understanding What is a Coronary Artery Calcium Score Matters for Heart Health
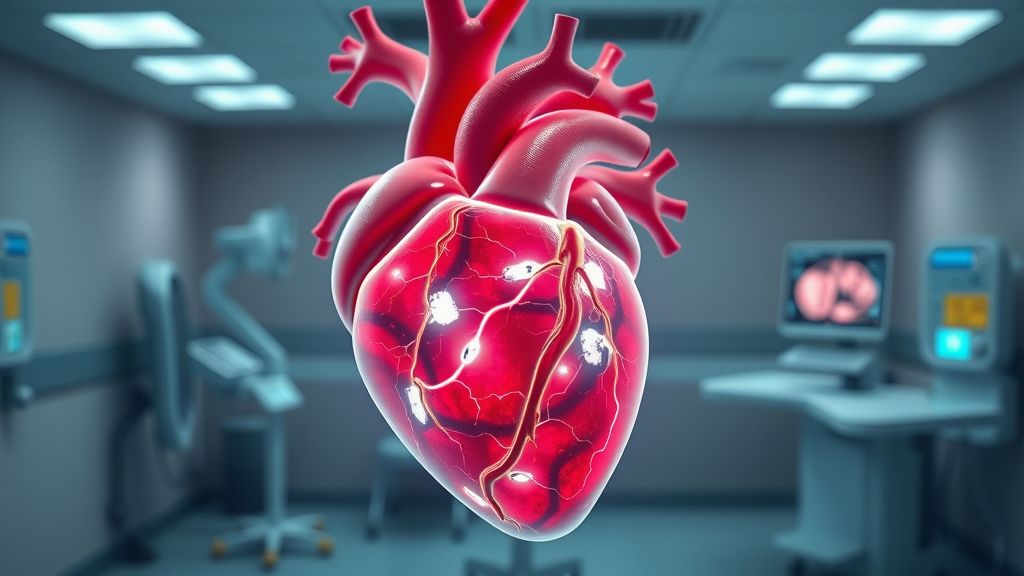
Knowing what is a coronary artery calcium score is increasingly seen as essential in the fight against heart disease. As the leading cause of death worldwide, heart disease often lurks without warning. Traditional risk factors such as high cholesterol, hypertension, and family history only paint part of the picture. Now, with modern technology, the calcium test offers a window into your arteries long before you ever feel chest pain or notice symptoms. A simple, non-invasive heart scan—specifically a CT scan—can tell you if you have dangerous artery calcium building up silently.
This kind of calcium scoring can help you and your doctor make actionable decisions before it’s too late. The value of the coronary artery calcium score lies in its ability to directly measure calcified plaque inside your coronary arteries, providing a clearer risk assessment for heart attacks or strokes than routine blood tests alone. Early detection with a coronary calcium scan empowers you to manage your cardiovascular risk, adjust your lifestyle, and potentially extend your life.
Did you know a coronary artery calcium score can predict your risk of heart disease years before symptoms appear? Understanding this simple test could be key to preventing a heart attack and saving your life.
The coronary calcium scan stands out as a pivotal advance because it can detect coronary artery calcium long before the development of obvious symptoms. Even if you feel fine, this simple calcium test could reveal a hidden threat. A heart scan takes only minutes but can yield information that shapes your long-term treatment plan, guides your care provider, and potentially prevents serious events like a heart attack or stroke.
With easy access to this predictive technology, more people now have the opportunity to learn their calcium score early, giving them a head start on taking control of their heart health. The knowledge gained from understanding your coronary artery calcium score can be life-changing, making prevention a reality rather than a guesswork approach.
While understanding your coronary artery calcium score is crucial, it's equally important to recognize how other cardiovascular risk factors, such as high blood pressure, can influence your overall heart health. For a deeper look at effective strategies and common misconceptions about managing hypertension, you may find it helpful to explore the truth about high blood pressure management and how it fits into a comprehensive prevention plan.
What You’ll Learn About Coronary Artery Calcium Scores
Definition and purpose of a coronary artery calcium score
How the calcium test works and why it's performed
The role of heart scans and CT scans
Who should get a calcium scoring test
How to interpret your results
The limitations and risks of coronary calcium scans
Understanding What is a Coronary Artery Calcium Score
Definition of Coronary Artery Calcium and Calcium Scoring
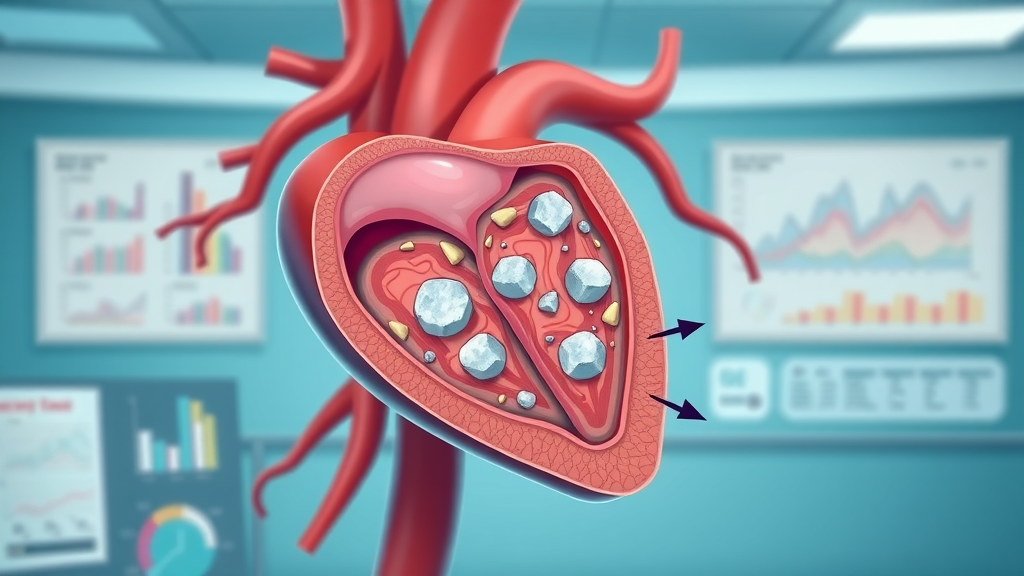
Coronary artery calcium (CAC) is the hardened, calcified plaque that builds up within the walls of your heart’s arteries. This calcified plaque is formed by a combination of cholesterol, fatty substances, and calcium over time. When your doctor orders a calcium test, also known as a coronary calcium scan or heart scan, they are trying to directly measure the extent of this build-up. Calcium scoring is the process by which your CT scan assigns a number to the amount of detectable calcium within the coronary arteries. This calcium score, also called a CAC score, ranges from 0 (no calcification) to several hundred—or even thousands—for those at high risk.
A CT scan (computed tomography) is central to this process because it provides crystal clear images of your coronary arteries, allowing doctors to spot calcium that would be invisible by other means. Knowing your artery calcium level is crucial, as studies show the amount of coronary artery calcium is a potent predictor of future heart attack or stroke. Essentially, the higher your calcium score, the greater your cardiovascular risk. This knowledge enables physicians and patients to catch impending heart disease before it triggers an emergency, making calcium scoring both revolutionary and preventative in modern medicine.
How a Calcium Test Indicates Hidden Heart Disease Risk
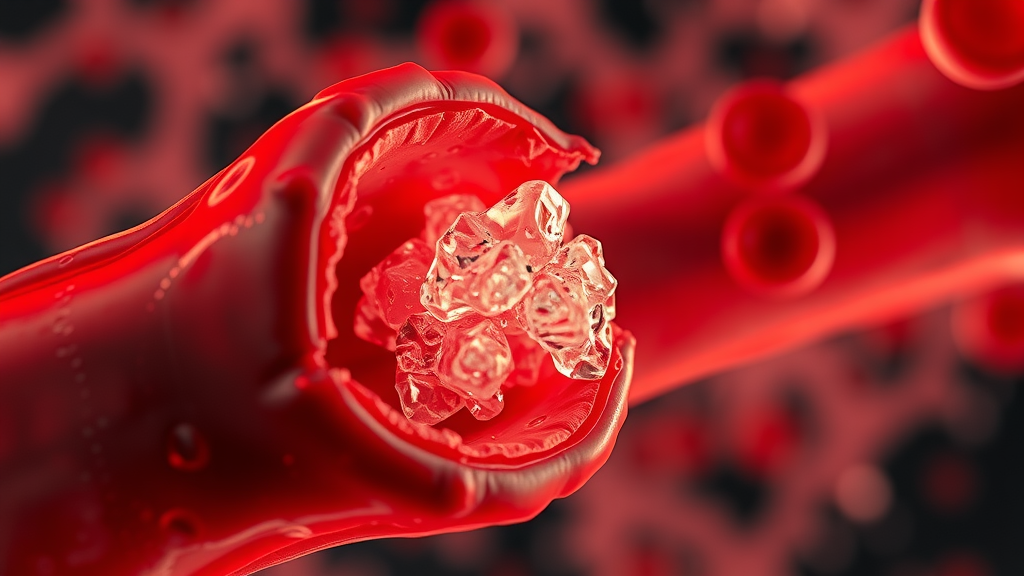
The coronary artery calcium score provides information about your risk of heart disease that other tests cannot. Unlike cholesterol or blood pressure measurements, a calcium scan pinpoints the actual presence of calcified plaque—a key marker for atherosclerosis. This means even people with normal cholesterol or no symptoms can harbor dangerous levels of artery calcium. If your calcium test uncovers moderate or high levels, it signals that you already have underlying coronary artery disease, even if you haven’t noticed any warning signs like chest pain.
Research has shown that people with a high CAC score have a dramatically increased risk of heart attacks or strokes compared to those with a low risk or zero score. The test’s value lies in how it motivates both patients and doctors to act early with medication, lifestyle changes, or further diagnostic testing. By identifying risk factors that might otherwise go undetected, the coronary calcium scan helps target aggressive preventive measures to those who need them most, tailoring care to the true threat lurking beneath the surface.
The Evolution of Heart Scan and CT Scan Technologies
Early efforts to evaluate coronary artery health relied primarily on indirect clues—symptoms, physical exams, and sometimes invasive tests. Today’s heart scan benefits from extraordinary advances in CT scan technology. Modern scanners use fast and low-dose x-rays to image the heart’s blood vessels with remarkably high clarity while minimizing the amount of radiation required. These improvements have dramatically increased the speed, accuracy, and safety of coronary calcium testing.
What was once reserved for patients with severe symptoms or after dangerous cardiac events is now part of a broader preventive strategy. Many hospitals and clinics offer coronary calcium scoring as an outpatient test requiring no recovery time. Its non-invasive nature, combined with the high predictive power, makes the calcium scan a frontline defense against cardiovascular disease. In the ongoing fight to reduce deaths from heart attack and stroke, technological evolution in heart scanning now gives patients a real edge in the race against time.

How the Coronary Artery Calcium Test Works
Step-by-Step: What Happens During a Coronary Calcium Scan
Preparation for a calcium scan: Typically, no special dietary or medication restrictions are required. But you may be asked to avoid caffeine or smoking beforehand to help slow your heart rate, ensuring clearer images during the calcium scan.
What to expect during the CT scan: You’ll lie comfortably on a table that slides into a CT scanner—a tunnel-like machine. Electrodes attached to your chest monitor your heartbeat. The scan is quick and painless; you may be asked to hold your breath for a few seconds to further stabilize your heart during the images.
Duration and safety: Most coronary artery calcium scans take just 10 to 15 minutes from start to finish, with the actual imaging lasting a minute or less. The amount of radiation is relatively low and considered safe for diagnostic purposes, especially given the potential to save lives by revealing hidden arterial plaque.
The Science Behind Calcium Scoring and Heart Disease
Why Coronary Artery Calcium is a Major Risk Factor
The build-up of coronary artery calcium within the vessel walls is not just a marker of aging; it’s a warning sign of atherosclerosis—the gradual narrowing and hardening of arteries that underpin most cases of heart attack and stroke. Unlike soft fatty plaque, calcified plaque is easily detectable with a calcium scan, making it an incredibly valuable indicator of overall cardiovascular risk. The direct measurement of coronary calcium provides unique insight into the health of your heart, revealing years’ worth of silent disease progression.
Research demonstrates that the amount of calcium present in the coronary arteries is strongly linked to a person’s risk of adverse cardiac events, independently of other traditional risk factors. The presence of artery calcium means that plaque build-up has already occurred over time, and this hardening typically signals a higher risk for obstructive disease. For this reason, many doctors now consider the coronary artery calcium score one of the best predictors of future heart attack or stroke risk, uniquely positioned to supplement cholesterol testing, blood pressure monitoring, and lifestyle assessments.
How the CAC Score Predicts Risk of Heart Attack or Stroke
A CAC score directly quantifies the amount of calcified plaque in the coronary arteries. Scores close to zero indicate little or no calcium and are considered low risk for heart attacks in the near future. As the score rises—to 100, 400, or even higher—the implication is that more extensive plaque build-up has occurred, substantially increasing your risk of heart attack or stroke. In fact, people with a high calcium score have several-fold greater risk of cardiovascular events compared to those with low or zero scores.
Doctors use this data to tailor prevention strategies. Someone with a zero or low CAC score may safely focus on lifestyle adjustments, while a patient with a high CAC score may benefit from more aggressive medical treatments, such as cholesterol-lowering medication or further diagnostic procedures. Understanding your coronary calcium scan results allows you and your care provider to make decisions based on actual disease burden rather than generic risk factors alone, making treatment both more precise and proactive.
Video explanation of the process of arterial calcification and its crucial connection to heart health and heart attack risk.
When Should You Get a Coronary Calcium Score?
Risk Factors That May Warrant a Calcium Test
Family history: If your parents or siblings had early heart attacks, your doctor might recommend a coronary calcium scan even if you don’t have symptoms.
High cholesterol: Elevated LDL cholesterol increases the risk of artery disease and atherosclerosis, warranting consideration for a heart scan.
Hypertension: High blood pressure accelerates plaque build-up in coronary arteries; a calcium test can quantify the danger.
Diabetes: Diabetes is a major risk factor for cardiovascular disease, often making a CT scan for calcium scoring a prudent screening step.
Age and gender: Men over 40 and women over 50, or post-menopausal women, are frequently in the age bands where risk for heart disease rises sharply.
Who is a Candidate for a Heart Scan?
Generally, individuals aged 40–70 with intermediate risk factors for heart disease are prime candidates for a heart scan. If you or your doctor are unsure about whether you need to start medication, a coronary artery calcium score can often provide that clarifying information. Those with a strong family history, high cholesterol, hypertension, diabetes, smokers, or former smokers are generally recommended for the CAC test. People without symptoms or those who do not have these risks generally may not benefit as much from the test, and it might not be routinely recommended.
If you've already had a heart attack, coronary angiogram, or have known coronary artery disease, your care provider may rely on different tests to monitor your progress. A calcium scan is most useful for uncovering hidden risks and helping to decide if lifestyle or medication changes are needed in those without known blockages.
Understanding and Interpreting Your Calcium Score Results
What Do Different CAC Scores Mean for Heart Health?
Interpreting your CAC score is crucial to understanding your risk of heart attack or stroke. The number you receive is more than just data; it represents the severity of existing coronary artery calcium, an indicator of your underlying risk for future cardiac events. Here’s a breakdown of standard calcium score ranges and what they mean:
Calcium Score Ranges and Their Interpretation |
||
Calcium Score (CAC) |
Interpretation |
Likely Risk |
|---|---|---|
0 |
No detectable calcium. Very low chance of significant coronary artery disease. |
Low risk |
1–99 |
Mild evidence of coronary artery calcium. Indicates early atherosclerosis. |
Mild risk |
100–399 |
Moderate coronary calcium deposits. Likely presence of significant plaque build-up. |
Moderate risk |
400 or higher |
Extensive coronary artery calcium. High likelihood of significant artery disease and increased risk of heart attack or stroke. |
High risk |
What is a Normal Coronary Artery Calcium Score?
A normal coronary artery calcium score is 0. This means that your heart scan did not detect any measurable calcium in the coronary arteries, indicating a low short-term risk of heart attack. People with a score of 0 typically do not need cholesterol-lowering medications unless other major risk factors exist. However, maintaining healthy habits, including staying active, eating a balanced diet, and avoiding smoking, is still important even when your calcium score is normal.
It’s essential to remember that a score of 0 does not mean your risk is zero for life. New plaque build can develop over time, especially if other risk factors change or worsen. The value of a zero CAC score is that it provides peace of mind about short-term risk and can help avoid unnecessary medications or procedures.
What is a Worrisome Calcium Score?
Generally, a worrisome calcium score is 100 or higher. As your score climbs above this level, it reflects a growing burden of coronary artery calcium and potential narrowing or blockage of the vessels. Scores above 400 significantly increase the likelihood of a heart attack or stroke, even if you don’t have symptoms. For most people diagnosed with high calcium, this news is a powerful motivator to take proactive steps.
High scores signal it’s time to work closely with your doctor to manage cholesterol, blood pressure, and other contributors to heart disease risk. Medical interventions such as statins, aspirin, or more advanced imaging may be considered to protect your heart and prevent complications down the line.
Beyond the Numbers: Limitations and Misinterpretations of Coronary Calcium Scanning
Can You Get False Positives or Negatives with Calcium Scoring?
While calcium scoring is a powerful tool, it’s not perfect. There are occasional false positives, where the calcium test shows build-up that doesn’t lead to a heart attack, or false negatives, where soft, non-calcified plaque remains undetected by a CT scan. Additionally, small amounts of calcium from non-coronary structures can sometimes be mistaken for coronary calcium, influencing your results.
Despite these rare inaccuracies, a coronary calcium scan correlates exceptionally well with real-world cardiovascular risk. However, no test is 100% predictive, so your personal risk and treatment decisions should always include input from your care provider and a careful review of all risk factors.
When Might a CT Calcium Scan Not Be Recommended?
There are situations where a coronary calcium scan isn’t helpful. Most obviously, it’s not recommended for people already diagnosed with coronary artery disease, previous heart attacks, or those with clear-cut symptoms that suggest severe obstruction. Pregnant women should not have the scan due to radiation exposure, and young adults without major risk factors do not usually benefit from testing.
If you’re unsure whether you need a heart scan, talk with your physician. They will help you weigh the benefits, risks, and timing, ensuring the test is used as part of a comprehensive prevention or diagnostic strategy.
How to Use Your Coronary Calcium Score for Better Heart Health
Lifestyle Changes to Lower Your Coronary Calcium Score
Diet and exercise: Adopting a heart-healthy diet low in saturated fats, rich in fruits, vegetables, and whole grains, complemented by regular physical activity, can slow or prevent further plaque build-up.
Cholesterol management: Keeping cholesterol and blood pressure under control via lifestyle and, if needed, medication, is vital for protecting against new calcium formation in the arteries.
Quitting smoking: Smoking accelerates coronary artery disease and calcification. Quitting reduces risk factors quickly, so seek help to stop if you smoke.

How Can I Lower My Coronary Calcium Score?
Though your calcium score itself may not decrease—since calcified plaque often remains visible on scans—taking action can dramatically reduce your risk of heart attack and stroke. Focus on lifestyle: Eat a plant-based, Mediterranean-style diet, exercise at least 150 minutes a week, manage stress, control your blood sugar if diabetic, and keep your blood pressure under 130/80 mmHg. Medications, such as statins, may be prescribed to slow the progression of new plaque and stabilize existing deposits, making them less likely to rupture and cause harm.
Speak to your doctor about ways to address all your personal risk factors. With a high CAC score, a proactive approach can help you live longer and healthier, even if the portions of calcium do not disappear.
Medical Interventions After a High Calcium Test
If your coronary artery calcium score is 100 or greater, your healthcare provider will likely recommend medication—even if your cholesterol isn’t very high. Statins, anti-hypertensives, and sometimes aspirin may be used. Advanced cases might require more detailed imaging or further evaluation for possible interventions. Your doctor can also help you manage other conditions such as diabetes or kidney disease, both of which increase the risk for cardiovascular events.
Collaboration with a cardiologist ensures that your treatment plan aligns with your values and unique situation. Monitoring repeat CAC scores is not generally needed unless your risk profile changes or new symptoms develop. The initial result is most important for long-term planning and prevention.

What Not to Do Before a Coronary Calcium Scan
Ask your doctor if you should pause any medications—most do not need any adjustment.
Avoid caffeine and smoking on the day of the scan. Both can raise your heart rate, interfering with image clarity.
Some facilities request you refrain from eating for a few hours beforehand, but fasting is not always essential. Always follow your doctor’s instructions.
FAQs About What is a Coronary Artery Calcium Score
Is a coronary calcium scan painful?
No, a coronary calcium scan is completely painless. You simply lie on a table while the CT scan images your heart. There are no needles or injections, and the test is over in minutes.How is the procedure different from other heart tests?
A coronary calcium scan is different from stress tests or angiograms because it directly measures the calcium in your arteries using a low-dose CT scan. Unlike stress tests, it doesn’t assess how well blood flows under exertion, but it is more specific in measuring calcified plaque build-up.How often should you have this test?
Most people only need one coronary calcium scan unless their risk factors change significantly or new symptoms develop. Your doctor will advise on whether repeat scans are necessary.Will insurance cover a coronary artery calcium scan?
Coverage varies by provider and location. Some insurance plans cover the test for those with intermediate or high risk, but others may not. It’s important to check with your insurer and your care provider before scheduling the scan.
Expert Insight on Calcium Test and Coronary Artery Health
"A coronary artery calcium score is one of the most precise predictors we have for future heart attack or stroke risk. It empowers patients and clinicians to make data-driven decisions." – Dr. Sarah Lee, Cardiologist
Key Takeaways About What is a Coronary Artery Calcium Score
Calcium scoring is essential for detecting hidden heart disease risks.
Not everyone needs it, but those with risk factors can benefit significantly.
Discussing results with a healthcare provider leads to better preventive care.
Conclusion: Taking the Next Step with Your Calcium Score
If you’re concerned about your heart health, discuss a coronary artery calcium score with your physician to see if this powerful test is right for you.
Understanding your coronary artery calcium score is a powerful step toward proactive heart health, but it’s just one piece of the cardiovascular puzzle. If you’re interested in broadening your knowledge about other key contributors to heart disease, such as cholesterol, consider exploring common cholesterol misconceptions and the facts behind them.
Gaining a well-rounded perspective on all major risk factors empowers you to make smarter choices and work with your healthcare provider on a truly comprehensive prevention strategy. The more you understand about the interplay between cholesterol, blood pressure, and calcium scoring, the better equipped you’ll be to protect your heart for years to come.
Sources
A coronary artery calcium (CAC) score is a measurement obtained through a specialized heart scan that assesses the amount of calcified plaque in your coronary arteries. This score helps predict your risk of heart disease and can guide treatment decisions.
For a comprehensive understanding of the CAC test, including its purpose, procedure, and implications, you can refer to the American Heart Association’s resource titled “Coronary Artery Calcium Test.” This article provides detailed information on how the test is performed and how the results can influence your heart health management. (heart.org)
Additionally, the Mayo Clinic offers an in-depth overview in their article “Coronary calcium scan,” which explains the significance of calcium scores and their role in assessing heart disease risk. (mayoclinic.org)
If you’re serious about understanding and managing your heart health, these resources will provide you with valuable insights into the importance and interpretation of coronary artery calcium scores.
Find tons more helath and wellness information on: https://ncwellnesshub.com/
 Add Row
Add Row  Add
Add 




Write A Comment