When Marie first felt knee pain, simple tasks became challenging. Through gentle beginner exercises designed for knee osteoarthritis, she regained strength and mobility safely. This article shares how you can start too, easing pain and improving your quality of life with easy, effective movements.

Introduction to Beginner Exercises to Manage Knee Osteoarthritis
Knee osteoarthritis is one of the most common causes of joint pain among adults, often making daily activities like walking, standing, and climbing stairs difficult. If you’re just beginning to explore ways to relieve arthritis pain in your knees, gentle movement can offer hope and real results. This guide focuses on beginner exercises to manage knee osteoarthritis safely. By building new habits, you may reduce pain, preserve mobility, and live with less discomfort—starting from home, at your own pace.
Understanding why exercise is essential and reviewing safe options is the first step toward reclaiming comfort and confidence. Even if you’ve never exercised before or have concerns about hurting your knee further, you’ll find practical and achievable movements that put safety and effectiveness first. Let’s discover how tailored, low-impact exercises for knee arthritis can change your daily life.
Understanding Knee Arthritis and Its Daily Impact
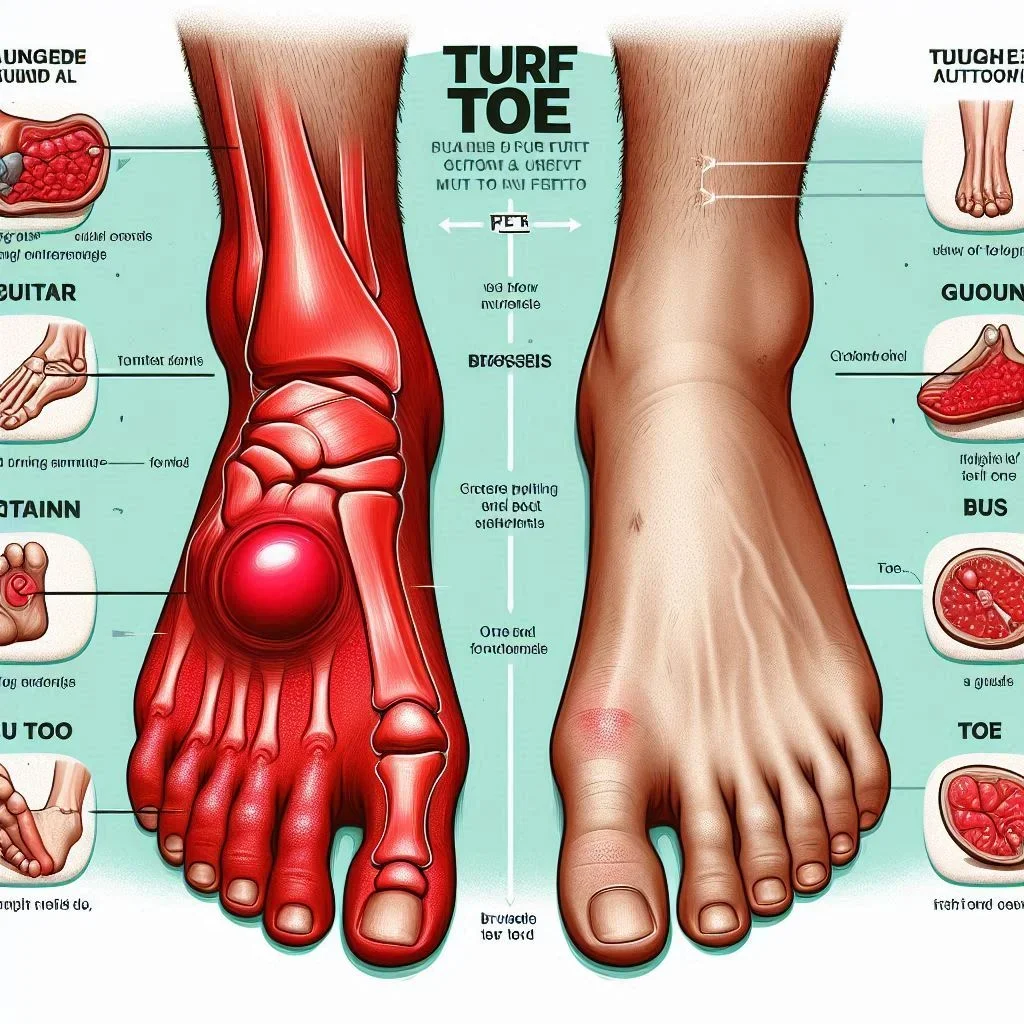
Knee arthritis, especially osteoarthritis of the knee, affects people of all backgrounds and ages but is most common as we get older. Cartilage in the knee joint—the protective tissue that cushions bone—wears down over time, leading to inflammation, stiffness, and chronic pain. Everyday movements like rising from a chair, walking short distances, or standing with knees bent can spark discomfort. The result? Many people withdraw from movement, which unfortunately can make things worse by weakening the leg muscles that support the knee.
This cycle of inactivity and rising discomfort emphasizes the need for beginner exercises to manage knee osteoarthritis. Targeted movements strengthen thigh muscles and improve the knee’s range of motion, making it easier to return to normal routines. Living with knee arthritis may feel discouraging, but gentle exercises are one of the clearest ways to take control and break the pain-inactivity cycle. Research shows that even a small increase in muscle strength and joint flexibility can lead to a noticeable reduction in arthritis pain and better function in daily activities.

The Importance of Safe, Low-Impact Exercise for Knee Osteoarthritis
When dealing with arthritis of the knee, it’s crucial to start slow and choose the right exercises. High-impact exercises like running or jumping can increase knee pain and cause more wear on the joint, making the symptoms worse. The best beginner exercises for knee arthritis focus on low-impact movement—think activities that keep both feet in contact with the ground or use smooth, controlled motions. These movements help build strength in the thigh and leg muscles without straining an arthritic knee.
Low-impact exercises for knee osteoarthritis can help reduce joint pain, enhance stability, improve flexibility, and increase overall muscle strength. By focusing on gentle movements such as straight leg raises, seated knee extensions, or water exercise, you avoid high stress on the knee, lowering your risk of further injury. Always listen to your body, and if any movement causes lasting pain, it’s a good idea to pause and consult a healthcare professional to adjust your routine for maximal safety and results.
As you build your beginner routine, you might also be interested in exploring other gentle exercise options that support joint health and overall mobility. For example, incorporating essential stretches for relieving sciatica pain can complement your knee osteoarthritis exercises by improving flexibility and reducing discomfort in the lower body.
Developing a Beginner Routine: Key Principles for Knee Arthritis

How Beginner Exercises Help in Managing Arthritis of the Knee
Starting a beginner exercise regimen can have a powerful effect on knee arthritis management. The first key benefit is combating muscle weakness; thigh muscle strength is directly tied to knee joint stability and function. Gentle moves like straight leg raises gradually build strength in these critical muscles, which in turn helps absorb shock and take pressure off the arthritic knee. Even small changes—increasing strength just a little—lead to better support for the joint during daily activities.
Another important aspect is maintaining or improving range of motion. Knee osteoarthritis often involves stiffness, which makes movement uncomfortable and can reduce joint health over time. Exercises that smoothly move the knee, like calf raises or gentle walking, can help “lubricate” the joint with synovial fluid. This fluid acts like oil, making movement easier and reducing pain during common tasks. With regular, safe practice, you can expect better mobility and less discomfort.
Straight Leg Raises and Their Role in Knee Health
Straight leg raises are one of the most recommended beginner exercises to manage knee osteoarthritis. This movement targets the quadriceps—the front thigh muscle group—without requiring you to bend the knee under load. Building these thigh muscles is crucial because they assist the knee joint as it bends, straightens, and supports your weight. The straight leg raise keeps joint impact to a minimum while reinforcing muscle strength and stability.
For those with knee arthritis, performing this exercise helps maintain the structural support of the knee and minimizes the risk of further arthritis pain during activity. By practicing straight leg raises regularly, you may notice improved knee stability and a reduction in knee pain during simple movements, such as getting up from a chair. Remember to switch legs to maintain balance and work both knees equally.
Step-by-Step Guide: Performing Straight Leg Raises for Knee Arthritis

Lie flat on your back, keeping one leg bent with the foot flat on the floor and the other leg straight.
Tighten your thigh muscle in the straight leg, slowly lift it about 12 inches off the floor. Keep your back straight and avoid arching.
Hold for a count of three to five, then slowly lower your leg back to the floor with control.
Repeat for 8-10 repetitions before you switch legs. Aim for two sets on each side. Always start slow and rest as needed.
"Safety should always be the priority. Start slow, listen to your body, and consult a healthcare provider before beginning new exercises for knee osteoarthritis." – Physical Therapist Jane Smith
Low-Impact Exercises for Knee Osteoarthritis: A Safe Starting Point

Why Impact Exercises are Not Recommended for Knee Arthritis
Impact exercises, such as running, jumping, and other high-impact aerobics, place a significant load on the knee joint, which is especially risky for people with arthritis of the knee. The jarring force travels through the joint, potentially aggravating inflammation, increasing knee pain, and accelerating cartilage wear and tear. Even if high-impact workouts feel effective in the short term, they often do more harm than good for knee arthritis.
Switching to low-impact exercises is a good idea for managing arthritis pain and reducing the risk of further injury. By choosing movements that avoid sudden shocks or excessive bending of the knee, you protect the joint and preserve mobility. Always prioritize slow, controlled actions that allow you to check your form and alignment—a principle recommended by physical therapists and the Arthritis Foundation alike.
Top Low-Impact Exercises to Manage Knee Osteoarthritis
Gentle Walking
Seated Knee Extensions
Calf Raises
Heel Slides
Mini Squats (with support)

Each of these exercises for knee arthritis specifically targets muscle groups around the joint, helps improve range of motion, and is designed to minimize impact. For example, gentle walking is accessible and can be tailored to your pace, while seated knee extensions activate the thigh muscle with very little strain on the joint. Calf raises and heel slides further support flexibility and muscle strength. If you choose to do mini squats, always use a chair for balance and keep knees bent only slightly—with no deep squatting—to remain safe.
Range of Motion Exercises for Knee Osteoarthritis
Increasing Flexibility and Reducing Stiffness
Improving your knee’s range of motion is fundamental in fighting stiffness and maintaining quality of life with knee osteoarthritis. Stiff joints can restrict your day-to-day movements and make activities like standing up, walking, or going up stairs more difficult. Incorporating range of motion exercises—such as gentle knee bends, flexion, and extension—helps stimulate production of synovial fluid, the lubricant of the knee joint. This natural lubrication not only reduces pain but also makes motion smoother and easier.
Popular exercises like gentle heel slides or hamstring stretches specifically target flexibility. Stretching the leg muscles—especially the back leg muscles—keeps calves, hamstrings, and thighs supple and supports the knee’s motion. Always start slow, avoid bouncing, and regularly switch legs to build balanced flexibility on both sides. A consistent routine can prevent long-term stiffness and help sustain your independence for daily activities.

Sample Routine: Morning Range of Motion for Arthritis of the Knee
Starting your day with a simple, gentle sequence can prime your knees for comfort and mobility. A good morning routine might include:
Sit at the edge of a sturdy chair with feet flat. Slowly extend one leg forward, straightening the knee as much as comfortable.
Lower your leg back down and repeat with the other leg. Complete 8 repetitions on each side.
Follow with gentle heel slides: Lie on your back, bend one knee, and slide the heel toward your hips before extending again.
Finish with a soft hamstring stretch: With a straight leg on the floor, lean forward gently until you feel a stretch behind the knee—never force or bounce.
Doing these exercises at the same time each day helps ingrain them as a healthy habit to reduce arthritis pain and stiffness.
Building Strength Without Stress: Resistance Beginner Exercises to Manage Knee Osteoarthritis

Using Bands and Bodyweight Safely
Building muscle strength around the knee doesn’t require heavy weights or gym machinery. Using a simple resistance band or your own bodyweight can effectively strengthen thigh and leg muscles critical for knee health. These beginner exercises are safe to do at home and allow you to control the intensity so you do not strain an arthritic knee. Examples include resistance band leg presses, bodyweight calf raises, and sitting-to-standing exercises while keeping the back straight.
Always ensure you’re using steady, controlled motion. Never jerk or force your way through a movement—this could harm the knee joint or cause unnecessary pain. Position a chair for balance if needed, and use the resistance band’s lightest setting at first. Over time, as strength improves, gently increase resistance and repetitions while monitoring your body’s response. If you notice any sharp or worsening knee pain, stop and adjust your approach, seeking guidance from a healthcare professional if needed.
Progressing Your Exercises for Knee as Strength Improves
It’s natural to want faster progress, but with knee arthritis, consistency and controlled progression are your best allies. Start with 8-10 repetitions of each exercise at a light intensity, two to three times per week. As your muscle strength builds, incrementally add repetitions or another set.
Gradually increase band resistance or incorporate more challenging exercises, like standing on one foot for balance or adding light weights—but only if you feel comfortable. Document your exercise routine in a journal to monitor improvements and recognize when you switch legs or increase difficulty.
-
Important Tips: Frequency, Repetitions, and Monitoring Pain
Begin with lower frequency (2–3 times per week) and slowly increase as tolerated.
Track your repetitions and sets; more is not always better—focus on quality of movement.
Monitor your pain. Minor discomfort is normal, but avoid exercises that result in lasting or sharp joint pain.

Combining Balance and Coordination with Beginner Exercises to Manage Knee Osteoarthritis
Simple Standing Balance Drills
Balance drills are often overlooked but are essential for preventing falls and enhancing confidence in daily movement for people with knee arthritis. For a safe, beginner-friendly drill, stand near a countertop or sturdy chair. With your feet hip-width apart, gently shift weight onto one leg while keeping your back straight and knees slightly bent; raise the other foot an inch or two off the floor and hold for several seconds. Repeat and switch legs, aiming for two or three sets of 5–10 seconds per leg, gradually increasing the duration as balance improves.
Make sure you always have support nearby, such as a countertop or wall, especially when first attempting these drills. Improving coordination and stability not only supports the knee but also builds confidence when walking outdoors or moving around the house.

The Role of Core Strength for Arthritis of the Knee
Many people are surprised to learn that core muscle strength directly influences knee health. A strong core helps maintain better overall posture and alignment, reducing compensatory strain on the knees. Simple core exercises, such as seated marches, gentle abdominal contractions, or modified planks, can be completed at home and are a good idea for those with knee arthritis looking to protect the joints and improve balance.
Building this muscle strength takes time, but the returns are significant: less joint pain, better stability, and even more effective results from other beginner exercises. Remember, start slow, use proper form, and consult a physical therapist if you want personalized suggestions that fit your current capacity and long-term goals.
This video features a certified physical therapist guiding you through essential beginner exercises to manage knee osteoarthritis. Learn proper form, pacing, and important safety cues for each movement. Visual reminders help you avoid common mistakes while highlighting smart ways to progress without risking joint pain.
Tracking Progress: Using a Table to Monitor Your Knee Arthritis Exercise Routine
Exercise Name |
Repetitions |
Sets |
Frequency |
Pain Level Rating |
|---|---|---|---|---|
Straight Leg Raise |
10 |
2 |
3x/week |
2/10 |
Seated Knee Extension |
10 |
2 |
3x/week |
1/10 |
Heel Slides |
12 |
2 |
4x/week |
2/10 |
Mini Squats |
8 |
2 |
2x/week |
3/10 |
Calf Raises |
15 |
2 |
3x/week |
1/10 |
Common Mistakes to Avoid During Beginner Exercises for Knee Osteoarthritis
Skipping Warm-Up
Doing High-Impact Exercises
Neglecting Alignment and Form

"Consistency beats intensity: Gentle progress is key in exercises for knee arthritis." – Orthopedic Surgeon Dr. Patel
People Also Ask
What is the most effective exercise for knee osteoarthritis?
Experts typically recommend straight leg raises and gentle walking as two of the most effective beginner exercises to manage knee osteoarthritis, as these improve strength and mobility with minimal stress on the joints.
What exercises should I avoid with osteoarthritis of the knee?
Exercises involving jumping, running, or sudden twisting, such as high-impact aerobics and deep squats, should be avoided with arthritis of the knee as they can aggravate pain and accelerate joint damage.
How to start exercising with osteoarthritis?
Begin with low-impact, basic movements, warm up thoroughly, and increase duration as tolerated. Consult your doctor before starting and build in rest days to prevent overuse.
What exercises lubricate the knees?
Range of motion exercises, such as gentle knee bends and extensions, help stimulate synovial fluid, which lubricates the joint and reduces stiffness associated with knee arthritis.
Watch this expert-led demonstration for tips on increasing intensity, adding new exercises, and ensuring each movement supports your arthritic knee as your strength improves.
Frequently Asked Questions: Beginner Exercises to Manage Knee Osteoarthritis
Is it safe to exercise every day with knee osteoarthritis?
Most people benefit from regular activity, but daily exercise may be too much for some. Aim for 3–5 days a week, including rest days for recovery. Listen to your body and adjust frequency if pain increases.How long until I notice improvement from beginner exercises?
Improvements in pain and joint function can often be seen in as little as 2–4 weeks, but this varies by individual. Consistent, gradual progress is most important for lasting results.Can I do these exercises if I have severe arthritis of the knee?
If you have severe arthritis, begin with the gentlest exercises, such as seated or lying movements. Always consult with a healthcare provider or physical therapist for a routine customized to your limitations and needs.
Key Takeaways: Beginner Exercises to Manage Knee Osteoarthritis

Gentle, regular movement can ease pain and improve knee function.
Start with low-impact, easy-to-follow exercises and progress gradually.
Listen to your body and consult a professional when needed.
Conclusion: Taking the First Step Toward Managing Knee Osteoarthritis
By adopting safe beginner exercises to manage knee osteoarthritis, you can regain mobility, comfort, and confidence in daily activities. Reach out to a healthcare provider to personalize your routine and ensure ongoing safety and progress.

If you’re ready to take your wellness journey even further, consider how a holistic approach to movement can benefit your entire body—not just your knees. Exploring the best exercises for longevity and overall vitality can help you build a sustainable, energizing routine that supports healthy aging and long-term mobility. By integrating these broader strategies, you’ll empower yourself to stay active, independent, and thriving for years to come.
Sources
To further enhance your understanding and management of knee osteoarthritis through exercise, consider exploring the following resources:
“Easy Exercises for Knee Arthritis: Stretches, Raises, and More” (healthline.com)
This article provides a comprehensive guide to simple exercises, including stretches and leg raises, specifically designed to alleviate knee arthritis symptoms.
“Exercises for Knee Osteoarthritis and Joint Pain” (webmd.com)
This resource offers a visual slideshow demonstrating various exercises aimed at improving joint health and reducing knee pain associated with osteoarthritis.
If you’re committed to managing knee osteoarthritis effectively, these resources will equip you with practical exercises to enhance mobility and reduce discomfort. NCWellnessHub.com
 Add Row
Add Row  Add
Add 



Write A Comment