Choosing between biosimilars and biologics isn’t just a scientific debate—it impacts patient access, healthcare costs, and treatment outcomes. Understanding these differences empowers us to support more affordable, effective therapies, ultimately transforming lives and reshaping the future of medicine.

Understanding the Battle: Biosimilar vs Biologic — Why It Matters
The biosimilar vs biologic discussion is about more than just medical innovation; it’s about making life-changing therapies accessible to millions worldwide. As biologic drugs revolutionize treatment for conditions like cancer, rheumatoid arthritis, and diabetes, biosimilars are poised to make these breakthroughs more available and affordable.
Each choice in this space ripples across healthcare—affecting not only individual patient outcomes but also the sustainability of entire care systems. With healthcare budgets straining under the rise of specialty medicines, deciding between a biologic drug and its biosimilar counterpart could mean the difference between continuing critical treatments or facing financial hurdles.
A key distinction in the biologics and biosimilars battle lies in their origin and composition. Biologics are complex medicines produced by living organisms, while biosimilars are highly similar versions introduced after the original product’s patent expires. The Food and Drug Administration (FDA) ensures both meet high standards for safety and effectiveness.
Yet, the debate goes beyond molecular structure—it challenges our healthcare priorities, insurance coverage, and doctor-patient trust in newer biosimilar products. As this landscape grows, understanding how biosimilars compare to their reference biologics empowers patients, providers, and policymakers to make informed, confident choices about the future of medicine.
Opening Insights: How Biosimilar vs Biologic Decisions Impact Patients and Healthcare
Choosing between a biologic and biosimilar can feel complex, yet the implications are far-reaching. Biologic medicines, crafted from living cells, have paved new paths for treating chronic diseases where traditional drugs falter. However, their high cost often limits widespread use.
Enter biosimilars—highly similar but generally less expensive alternatives approved once original biologic patents expire. The FDA’s standards assure that biosimilars have no clinically meaningful differences in safety, purity, or potency, yet even subtle differences in manufacturing can raise questions among clinicians and patients.
This choice isn’t just about efficacy; it’s about equality in care. Patients benefit when competition drives down healthcare costs and broadens treatment options. Still, acceptance depends on trust—both in biosimilars’ safety and in regulatory processes assuring their safety and effectiveness. As we navigate new approvals and education efforts, the biosimilar vs biologic debate remains at the heart of access, cost, and quality in modern medicine.
While understanding the science behind biosimilars and biologics is crucial, it's equally important to recognize how these advanced therapies fit into broader health and wellness strategies. For those interested in optimizing overall well-being, exploring practical approaches to managing common health challenges, such as digestive comfort during pregnancy, can complement your knowledge of innovative treatments.

“Choosing the right therapy—biosimilar vs biologic—can alter treatment outcomes and system-wide healthcare costs.”
What You'll Learn: The Essentials of Biosimilar vs Biologic
Definition of biosimilars and biologics
Differences and similarities between biosimilars, biologics, and generic drugs
Regulatory and safety considerations
Cost implications for healthcare systems
Expert opinions and real-world impact
Biologics and Biosimilars: Breaking Down the Basics
Understanding the basics of biologics and biosimilars is key to making informed treatment choices. A biologic drug is developed from living organisms, such as bacteria, yeast, or animal cells. This makes their structure incredibly complex and sensitive to variations in the manufacturing process.
As a result, small differences, known as minor differences, can occur even in different batches of the same biologic. Despite this, all biologic products must meet rigorous standards set by the Food and Drug Administration to ensure they are safe and effective.
Biosimilars enter the scene as almost identical versions of existing biologic medicines, introduced once the original product's patent expires. The distinguishing factor is that biosimilars are designed to be highly similar to their reference product, but not exact copies.
Still, they undergo exhaustive comparison studies so any possible clinically meaningful differences in safety, efficacy, or immune system response are carefully ruled out. This process keeps patient safety at the forefront while allowing for increased competition and more affordable treatment options.

What is a Biologic Drug? Understanding Complex Medicines from Living Organisms
A biologic drug is any medical product derived from a living organism. Unlike traditional medicines made by simple chemical processes, biologics rely on complex biological processes involving living cells. These drugs can include proteins, monoclonal antibodies, and hormones used to treat a wide range of diseases, from rare genetic disorders to common autoimmune conditions.
Their molecular complexity and origin make biologic drugs distinct from chemically synthesized products and lead to unique characteristics—such as potential interactions with the immune system, variable side effects, and the need for special storage and administration.
Because the manufacturing process uses living organisms, even slight changes in technique, raw materials, or environmental conditions can affect the final biologic product. As a result, regulatory agencies like the FDA require extensive oversight to guarantee every batch is safe and effective. The goal is to make sure patients receive consistent, reliable treatment, even when medications come from incredibly complex sources.
What is a Biosimilar? From Reference Biologics to Patient Care
A biosimilar is a type of biological medicine that is highly similar to a reference biologic already approved by regulatory bodies. These therapies go through thorough studies to show that they have no clinically meaningful differences compared with the original biologic. To be approved, a biosimilar product must prove comparable purity, potency, and safety, and it must act in the body the same way as the reference biologic.
Developing a biosimilar starts by analyzing the original biologic—‘the reference product’—to match its specific structure and function as closely as possible. Scientists then use advanced biological manufacturing processes to create a comparable medicine. Rigorous laboratory and clinical studies ensure the biosimilar delivers the same benefits as its reference biologic, which provides doctors and patients with reliable and potentially cost-effective new treatment options.
How living organisms produce biologics
The development process of biosimilars
Biosimilar vs Biologic: Similarities, Differences, and the Generic Drug Comparison
When exploring biosimilar vs biologic distinctions, it's important to note that while both are made from living organisms and must be safe and effective, biosimilars enter the market after the reference biologic’s patent protection ends. This competitive process drives down costs and increases treatment options, but regulation and scientific scrutiny remain high. Biosimilars are not generic drugs; instead, they are more complex and must be highly similar—not identical—to their reference product, reflecting their biological origins.
In contrast, a generic drug is created to be a chemical copy of a brand-name medicine, matching it in active ingredient and dosage form, ensuring the same clinical result in patients. With biologics, the natural variability from using living organisms means biosimilars can only be similar, not identical. This makes the regulatory pathway for biosimilars more rigorous, focusing on comparative safety, effectiveness, and immunity. Still, like generics, biosimilars aim to provide affordable alternatives without clinically meaningful differences.

How Biosimilar vs Biologic Compares to Generic Drugs
One of the most common questions is how biosimilars differ from generic drugs. Generics are exact chemical copies of brand-name (innovator) drugs, offering identical active ingredients, strength, and administration. This means generics have straightforward, less costly approval pathways.
In contrast, biosimilars are developed from biologic medicines, which are far more complex and made using living organisms. Because the manufacturing process cannot completely duplicate the original biologic, biosimilars are only highly similar—not identical. This difference requires more advanced analytical techniques and strict clinical evaluations to show no clinically meaningful differences in effect or side effects. Ultimately, both biosimilars and generics expand access to critical medicines, but biosimilars undergo unique regulatory scrutiny because of their intricate makeup.
Comparison of Biosimilar vs Biologic vs Generic Drug Characteristics |
|||
Characteristic |
Biologic |
Biosimilar |
Generic Drug |
|---|---|---|---|
Source |
Living organisms |
Living organisms (based on existing biologic) |
Chemical synthesis |
Complexity |
Very high (proteins, antibodies) |
Very high, highly similar to reference |
Low, simple chemical structure |
Approval Path |
Full clinical trials |
Comparative studies to reference biologic |
Bioequivalence studies |
Interchangeability |
N/A |
Possible with FDA designation |
Generally automatic at pharmacy |
Cost |
High |
Lower than reference biologic |
Low |
Minor Differences |
Batch-to-batch variation |
Allowed if no impact on safety/effectiveness |
Not expected |
Reference Biologics and the Road to Biosimilar Approval
The original biologic product, also known as the reference biologic, sets the standard for biosimilars. When a manufacturer develops a biosimilar, it analyzes the reference product’s structure, biological activity, and clinical effects. Extensive lab and clinical studies assess whether the candidate biosimilar is highly similar with no clinically meaningful differences in terms of safety, purity, and potency. The process tests for immune system response, potential side effects, and ensures identical drug administration methods.
Only after meeting rigorous FDA requirements can a biosimilar be approved—and, in some cases, achieve “interchangeable” status, meaning pharmacists may substitute it for the reference biologic without consulting the healthcare prescriber. This road keeps patient safety paramount while encouraging innovation, affordability, and expanded treatment options in the rapidly evolving field of biologic medicines.
Developing Biologics and Biosimilars: From Living Organisms to Therapies
The journey from laboratory to pharmacy shelf begins with the science of living organisms. Biologics and biosimilars are produced using advanced biotechnology techniques where cells—often genetically engineered bacteria or animal cells—are “programmed” to manufacture therapeutic proteins. The manufacture of a biologic drug is drastically different from the simple chemical synthesis of traditional medicines; instead, it requires precise control of living systems and a highly regulated environment throughout every stage.
Once a biologic is approved using a full suite of clinical trials, biosimilars follow with advanced comparative assessments against the reference product. The biosimilar manufacturer must prove, through analytical and clinical studies, that its product behaves like the original in terms of safety, immune system impact, and efficacy. Strict adherence to quality, purity, and reproducibility ensures biosimilars are as safe and effective as their reference biologics, reinforcing patient and provider trust.
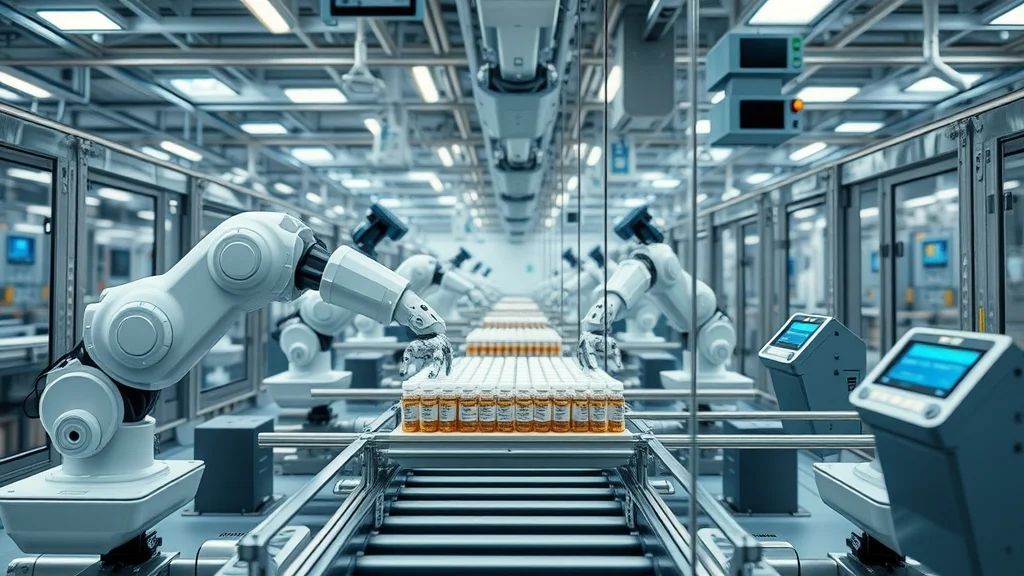
The Science of Living Organisms in Biologic Drug Manufacturing
Manufacturing a biologic drug is a biological feat—using living systems to produce drugs that are nearly impossible to synthesize chemically. Whether it’s monoclonal antibodies or recombinant hormones, the process starts by inserting a gene coding for the desired protein into a living cell. These cells are then grown in carefully controlled bioreactors, where they generate the complex molecules that become today’s most advanced medicines.
These unique methods result in biologic medicines with natural variability; it’s nearly impossible to make two batches exactly the same. This is why biosimilars can only be highly similar—and never exact copies—of their reference product. Consistency and quality are enforced through carefully regulated manufacturing and constant monitoring to prevent any clinically meaningful differences affecting safety or efficacy. It’s this intricate science of living cells that sets both biologics and biosimilars apart from simpler, traditional generic drugs.
Safety and Effectiveness: Regulatory Pathways for Biologics and Biosimilars
To ensure patient safety, the FDA and other regulatory bodies require extensive studies from both biologic and biosimilar manufacturers. For an original biologic, this means full clinical trials to prove it’s safe and effective for its intended use. For biosimilars, the regulatory pathway focuses on demonstrating that the new product is highly similar to the reference biologic and has no clinically meaningful differences in terms of safety, purity, or potency.
This assessment includes advanced laboratory analysis, animal studies, and human clinical trials—always with an unwavering focus on patient health and the potential for side effects or unique immune responses. These rigorous standards, developed by agencies like the Food and Drug Administration, ensure every biosimilar and biologic medicine brought to market meets modern standards for quality and patient care.
“Rigorous testing ensures both biosimilars and biologics remain safe and effective for all patients.”
Interchangeable Biosimilars: Expanding Options for Clinicians and Patients
A particularly innovative aspect of biosimilars is the designation of interchangeable biosimilars. When a biosimilar is proven to produce the same clinical result as its reference biologic for all approved uses—and to pose no additional risk in terms of safety or immune system effects when switching back and forth—it may earn “interchangeable” status from the FDA. This means a pharmacist can substitute an interchangeable biosimilar for its reference product, much as with generic drugs.
For clinicians and patients, this opens a new world of treatment options. It can help streamline prescribing, control healthcare costs, and improve access to safe and effective therapies—offering broader, affordable choices in chronic disease management.

What Makes an Interchangeable Biosimilar Safe and Effective?
Interchangeability is a special status confirmed by the FDA. To qualify, a biosimilar must not only show high similarity with no clinically meaningful differences to the reference biologic, but also pass switching studies—clinical trials that prove patients can change between the biosimilar and original biologic without new risks or reduced efficacy. This designation strengthens trust in biosimilars and makes it easier for providers and pharmacists to offer cost-saving alternatives.
In practice, interchangeable biosimilars expand affordable medication access. Patients can confidently transition to these options, knowing rigorous science and regulatory oversight ensure safety and effectiveness at every step.
FDA requirements for interchangeability
Clinical impact for patients and providers
The Economic Impact: Biosimilar vs Biologic on Healthcare Costs
The economic impact of adopting biosimilars is significant—both for patients and the larger healthcare system. Since the cost of biologics can be exceptionally high, introducing biosimilars immediately creates market competition, which has historically reduced prices and improved access. In therapy areas dominated by biologics, patients previously unable to afford advanced treatments now have more options. This aligns with the push for sustainable healthcare spending and ensures modern therapy is available to broader populations.
However, successful adoption requires buy-in from prescribers, payers, and patients. Misconceptions about the comparative safety and effectiveness of biosimilars versus biologics can slow acceptance, as can established contracts and insurance coverage policies. Yet, early data show biosimilars are already delivering meaningful savings, with some estimates projecting billions in annual healthcare savings when these therapies are fully embraced.
Biosimilars: Potential for Cost Savings and Increased Access
Biosimilars are uniquely positioned to drive down drug costs while maintaining—and sometimes even expanding—patient access to biologic medication. Because they are developed after a reference biologic’s exclusivity expires, manufacturers can offer biosimilars at lower prices due to reduced research and development expenses. This benefit is then passed on to patients and healthcare systems through lower out-of-pocket costs, broader insurance coverage, and less strain on medical budgets.
These savings do not come at the expense of quality; regulatory agencies ensure every biosimilar is safe and effective before approving its use in clinical practice. As biosimilars gain momentum, they hold enormous promise for making previously costly treatments accessible to many more people without sacrificing therapeutic outcomes.

Barriers to Adoption: Physician, Patient, and System Perspectives
Despite their benefits, biosimilars face several adoption hurdles. Many providers and patients are cautious, concerned about potential clinically meaningful differences or unfamiliar side effects. System-wide, insurers and pharmacy benefit managers must adjust formularies and reimbursement policies, a process that can be slow and complex.
Education is critical—when stakeholders understand the science and stringent regulatory standards behind biosimilars, acceptance grows. Furthermore, as more data accumulate demonstrating real-world safety and effectiveness, trust in these invaluable biosimilar products strengthens. Overcoming these barriers depends on collaboration between regulators, healthcare providers, patients, and industry leaders—all working to advance patient care through innovation and access.
“While biosimilars offer promise, stakeholder confidence is vital for broad adoption.”
Clinical Case Study: A Real-World Switch from Biologic to Biosimilar
To illustrate the real-life impact of biosimilar adoption, consider a patient with rheumatoid arthritis who has relied on a high-cost biologic for years. When a biosimilar alternative for their reference biologic becomes available, their rheumatologist recommends the switch, explaining that clinical trials confirmed no clinically meaningful differences in effectiveness or side effects.
Over time, the patient experiences no worsening in symptoms or additional immune system issues. Medication costs drop, making ongoing treatment affordable. This positive experience boosts their confidence in biosimilars and encourages others to explore these new treatment options. Such stories, increasingly common as biosimilars become more prevalent, highlight the practical benefits and promise these medicines offer for patients and healthcare systems alike.

People Also Ask About Biosimilar vs Biologic
What is the difference between biosimilars and unbranded biologics?
The key distinction lies in regulatory approval and naming conventions. Biosimilars are independently developed versions of an already approved reference biologic and must demonstrate high similarity with no clinically meaningful differences in safety, purity, or potency. Unbranded biologics, called "biogenerics" in some regions, may refer to off-patent biologics marketed without a brand name but not necessarily tested through the rigorous biosimilar pathway. Biosimilars undergo strict comparison to a reference product, while unbranded biologics may simply be relabeled versions of the original biologic.
Are biosimilars safer than biologics?
Biosimilars are required to demonstrate no clinically meaningful differences in safety and effectiveness compared to their reference biologic. They must pass comprehensive testing and regulatory review to be considered safe and effective. While not 'safer' than originator biologics, biosimilars are equally safe when approved and can even enhance safety monitoring due to modern manufacturing oversight.
Is Humira a biologic or biosimilar?
Humira (adalimumab) is a biologic drug. It was initially approved as an original reference biologic for treating autoimmune diseases. Now, several biosimilars for adalimumab have been developed and approved, offering patients more affordable alternatives with the same established safety and effectiveness.
Are biosimilars only for biologics?
Yes, biosimilars are by definition modeled after original biologic medicines. Unlike generic drugs, which are identical chemical copies of small-molecule drugs, biosimilars are only possible for complex medicines produced using living organisms due to their unique structures and production methods.

Frequently Asked Questions: Biosimilar vs Biologic
What conditions are treated with biosimilars and biologics?
Biologics and biosimilars are used to treat a range of diseases, including autoimmune conditions like rheumatoid arthritis, psoriasis, and Crohn's disease; cancers, including lymphoma and breast cancer; as well as hormonal deficiencies and rare genetic disorders. These therapies are often prescribed when conventional treatments do not provide sufficient benefit.How do insurance plans handle biosimilars vs biologics?
Insurance coverage varies. Many plans encourage biosimilar use by assigning lower copays when a less expensive biosimilar is available. However, formulary preferences, prior authorization requirements, and contracts with drug manufacturers can influence which product is covered for a specific condition. Patients should consult their insurer or care team for specifics.Can patients switch between biologic and biosimilar medicines?
Yes, under clinical guidance, patients can usually switch between a reference biologic and its approved biosimilar as studies show no clinically meaningful differences in safety or efficacy. The switch should be managed and monitored by the healthcare provider to ensure optimal outcomes and minimize any potential side effects.
Expert Opinions and Future Trends in Biosimilar vs Biologic Medicines
Experts agree that the future of biologics and biosimilars is one of rapid growth, global collaboration, and ongoing innovation. Robust regulatory frameworks and transparent education for providers and patients will underpin continued success. As more biosimilar products reach the marketplace, the emphasis will shift to real-world data, updating clinical guidelines, and expanding access—especially in underserved regions. Many anticipate that advances in biotechnology and regulatory science will make biosimilars an equally trusted element alongside original biologics.
International efforts are also underway to harmonize biosimilar approval standards, opening the door for worldwide access to advanced therapies. As the field evolves, it is clear that biosimilars and biologics together will remain central to tackling chronic disease, improving patient lives, and ensuring the long-term sustainability of global health systems.
"The future of biosimilar vs biologic medicines lies in global collaboration, robust regulation, and patient education."

Key Takeaways from the Biosimilar vs Biologic Debate
Biosimilars and biologics are both vital for modern healthcare
Biosimilars offer competitive options in cost and access
Safety and efficacy are closely monitored by regulators
Ready to Learn More? Connect with Biotech Experts for Latest Biosimilar vs Biologic Updates
Staying informed about the evolving world of biosimilar vs biologic medicines is essential. For updates, detailed guidance, or to speak with biotech specialists, reach out to trusted healthcare providers or visit official regulatory and patient advocacy sites for the most recent, reliable information.
Conclusion
Biosimilars and biologics, together, are reshaping patient care for the better—balancing innovation with access, and offering real hope for more affordable, effective health solutions.
If you’re inspired to take a more holistic approach to your health journey, consider how advancements in biotechnology can complement other wellness strategies. For example, integrating evidence-based exercise routines can support overall vitality and resilience, especially as we age.
Discover how simple resistance band exercises tailored for older adults can enhance strength and mobility—empowering you to make the most of modern medical breakthroughs and everyday healthy habits alike. Exploring these resources can help you build a well-rounded foundation for lifelong wellness.
Sources
Understanding the distinctions between biosimilars and biologics is crucial for informed healthcare decisions. The FDA’s article, “Biosimilars Basics for Patients,” provides a comprehensive overview, explaining that biosimilars are highly similar to their reference biologics with no clinically meaningful differences in safety or effectiveness.
In Addition, the American Cancer Society’s piece, “Biosimilar Medicines,” delves into how these medications are developed and their role in cancer treatment.
Exploring these resources will enhance your understanding of how biosimilars and biologics compare, aiding in better healthcare choices. NCWellnessHub.com
 Add Row
Add Row  Add
Add 



Write A Comment