Wondering if your symptoms mean a simple stomach bug or serious food poisoning? Understanding the timeline of onset for stomach flu and food poisoning can reveal the truth and guide your next steps for effective treatment. Are you ready to decode your body's signals and take control of your recovery? This comprehensive guide will empower you with the latest research, expert advice, and practical tools to confidently identify and respond to stomach bug or food poisoning issues.

Decoding the Stomach Bug or Food Poisoning Dilemma with the Timeline Test
When your day is interrupted by sudden nausea, vomiting, or stomach cramps, it’s natural to wonder: do you have a stomach bug or food poisoning? While stomach flu (viral gastroenteritis) and food poisoning share common symptoms such as abdominal pain, watery diarrhea, and fever, their key differences in causes and onset timelines make accurate self-diagnosis challenging. The key is understanding the timeline test, which can help you distinguish between these common ailments, ensure you take correct actions, and reduce potential complications.
In a world where food safety and infectious outbreaks are real concerns, being informed is not just a good idea—it’s essential. In this guide, we’ll tackle the symptoms of food poisoning and stomach bugs, explain why the onset and duration matter, and teach you when to seek urgent care or primary care based on expert-backed red flags.
Understanding Stomach Bug or Food Poisoning: Why the Timeline Matters
Both stomach flu and food poisoning can cause similar gastrointestinal distress, but the poisoning and the stomach flu differ significantly in sources and incubation periods. Food poisoning often hits hard and fast, sometimes within hours after contaminated food, while stomach flu or viral gastroenteritis may take a day or more before symptoms arise. The timeline—how soon after exposure you start feeling sick—offers a crucial clue for differentiating between the two.
Recognizing these distinctions helps prevent foodborne illness complications and guides safer, more effective recovery choices for you and your family. That’s why medical experts like Dr. Natalie Chen emphasize the importance of tracking the timeline from first exposure to symptoms. In the United States, millions experience vomiting and diarrhea each year, but understanding the timeline puts control back in your hands.
In addition to understanding the timeline, it's also important to recognize how underlying digestive conditions can influence your risk and recovery. For example, individuals with chronic gut issues such as IBD may experience more severe symptoms or complications.
If you're curious about how alternative therapies like cannabis might impact gut health and inflammatory bowel disease, explore the evidence on cannabis and IBD management for a deeper look at emerging research and practical considerations.
How to recognize the difference between food poisoning and stomach bug
Key symptoms of each condition and their warning signs
The timeline test: what it is and how to use it
Critical risk factors and who’s most at risk for complications
Home remedies and evidence-based recovery tips
When to seek urgent care or consult a healthcare provider
Stomach Bug vs. Food Poisoning: Common Symptoms and Early Warning Signs
Distinguishing between stomach flu and food poisoning can be challenging due to their common symptoms, but recognizing the key differences in onset and severity is essential. Rapid onset of abdominal pain, diarrhea, vomiting, and feelings of queasiness are hallmarks for both issues. However, certain key differences—especially in how quickly symptoms appear—offer important clues that help direct your care. Both viral gastroenteritis and foodborne illness are highly contagious, affecting individuals of all ages.
Tracking the appearance and pattern of initial symptoms, as well as noting exposure to recent contaminated food or sick contacts, can enhance early recognition. In many cases, recognizing these early warning signs can help you take prompt action—reducing illness severity and decreasing chances of spreading infection to others.
Early symptoms of food poisoning may include intense abdominal cramping and a sudden urge to vomit, often within a few hours of eating contaminated food. On the other hand, the stomach flu may begin with mild discomfort and evolve into vomiting and diarrhea over the course of a day.
It’s also worth noting that some symptoms, like high fever with food poisoning, are less common but can indicate a more severe infection. Recognizing the subtle variations in symptom presentation and timeline not only aids a correct at-home diagnosis, but also ensures you seek timely help if complications arise.

Common symptoms of a stomach bug (stomach flu): Nausea and vomiting, watery diarrhea, mild to moderate fever, abdominal cramps, headache, and muscle aches.
Common symptoms of food poisoning: Sudden severe abdominal pain, vomiting and diarrhea (sometimes bloody), fever, chills, fatigue, and occasionally neurological effects in severe cases.
Stomach Flu vs. Food Poisoning: Key Differences in Onset Time and Severity
Understanding the key differences in onset and duration between stomach flu and food poisoning is fundamental for effective treatment and prevention. Typically, food poisoning strikes quickly—sometimes as soon as 1-6 hours after eating contaminated foods, especially those with strong toxins or bacteria like Staphylococcus or Salmonella. The symptoms of food poisoning can come on suddenly and may be more severe in the first 24 hours.
In contrast, a stomach bug often has a longer incubation period. For instance, viral gastroenteritis caused by norovirus may not present symptoms until 24-48 hours after exposure. While both conditions can have overlapping signs such as nausea and vomiting, food poisoning tends to resolve faster (within 12-48 hours for mild cases), although severe cases can last longer.
*Stomach flu typically resolves in 1-3 days, but fatigue may linger. These key differences underscore why paying attention to the timing of symptoms is so important, especially when seeking the right care.
Severity also varies. While most cases of either condition are self-limited, food poisoning has the potential to cause more serious complications like dehydration, kidney damage, or neurological symptoms if specific toxins are involved. Both conditions require careful monitoring, especially for high-risk groups like young children and elderly adults.
Being able to distinguish symptoms of food poisoning and stomach bug based on onset and severity increases your ability to respond quickly and appropriately—something every family medicine provider advocates.
Timeline Comparison Table: Stomach Flu vs. Food Poisoning Onset, Duration, and Severity
Feature |
Stomach Bug (Stomach Flu) |
Food Poisoning |
|---|---|---|
Incubation time (from exposure to first symptoms) |
12–48 hours (sometimes longer depending on virus) |
1–6 hours (preformed toxins); 6–48 hours (bacterial/viral) |
Onset pattern |
Gradual: mild discomfort, then nausea & diarrhea |
Sudden: severe vomiting, intense abdominal pain |
Duration |
1–3 days, sometimes longer with fatigue |
12–48 hours (most cases), up to 7+ days (severe cases) |
Severity |
Mild to moderate, rarely life-threatening |
Variable; can be severe, esp. with dehydration |
Contagious? |
Highly contagious (person-to-person, surface contact) |
Usually not, unless some viruses; spread by food/water |
The Timeline Test: How to Tell if It’s Stomach Bug or Food Poisoning
The timeline test is a crucial method for distinguishing between stomach flu and food poisoning by analyzing symptom onset after exposure. By tracking the window between exposure and the onset of symptoms, you can make an educated guess as to which illness you’re facing. For example, if symptoms appear within a few hours of eating, especially after a questionable meal, food poisoning is the likely culprit. Conversely, if discomfort starts more than a day after contact with a sick person or contaminated surface, a stomach bug (viral gastroenteritis) is more probable.
Not only does this test help with early identification, but it can also dictate what steps to take next. For instance, prompt hydration is crucial in both cases, but people with food poisoning need to monitor for signs of severe dehydration or blood in stool. The timeline test is therefore a good idea not just for personal clarity, but as a preventive measure, especially during outbreaks or when traveling. Remember to document potential exposures, what you ate, and key symptom changes to share during your primary care or urgent care visit if symptoms persist.
Case Study: Real Timelines of Patients with Stomach Flu and Food Poisoning
To better understand the timeline test, consider these real-world patient scenarios.
Case 1: A college student attends a family barbecue and eats potato salad that was left in the sun. Within 4 hours, he develops intense stomach cramps, vomiting, and watery diarrhea—classic signs of food poisoning due to rapidly acting staphylococcal toxin. He requires oral rehydration and recovers within 24 hours.
Case 2: A preschool teacher’s child has been fighting a fever and vomiting. About 36 hours after cleaning up the child’s mess, she starts to feel tired, then develops chills, nausea, and finally diarrhea—pointing to a stomach bug contracted from close contact. Her symptoms peak over two days and gradually resolve with rest and fluids.
These cases illustrate the predictive value of the timeline test. As Dr. Natalie Chen, Board-Certified Emergency Physician, notes:
"The timeline from exposure to symptoms is one of the most reliable clues for distinguishing between a stomach bug and food poisoning." — Dr. Natalie Chen, Board-Certified Emergency Physician
Watch:
What Causes Stomach Bug or Food Poisoning? Pathogens and Risk Factors
The underlying causes of stomach flu and food poisoning involve various pathogens, with distinct risk factors influencing each condition. Food poisoning generally stems from eating or drinking contaminated food or water. Bacteria like Salmonella, E. coli, and Campylobacter are common culprits, but viruses and parasites can also play a role.
Meanwhile, viral gastroenteritis—the stomach bug—is usually caused by viruses (norovirus, rotavirus) spread via close person-to-person contact, contaminated surfaces, or occasionally food/water. Recognizing the source not only aids with timely intervention, but also helps prevent food poisoning and the spread of stomach flu at home and in communities.
Risk factors include travel to areas with poor sanitation, consuming undercooked or raw foods, improper food storage, and poor hand hygiene. Certain populations, such as young children and people with compromised immune systems, have higher risk for severe illness from both conditions. Frequent handwashing and safe food practices remain foundational for prevention.
In the United States, foodborne illness and stomach bugs account for millions of lost work and school days annually—highlighting the importance of environmental hygiene and personal safety practices like washing your hands before eating or after using the restroom.

Stomach Bug vs. Food Poisoning: Key Differences in Transmission and Risk
Though stomach flu and food poisoning share common symptoms, their transmission methods differ significantly, impacting personal risk and public health strategies. Stomach bugs (viruses) are typically highly contagious and often spread between people through close contact, airborne droplets (from vomiting), contaminated surfaces (toys, bathroom handles), and even by touching your face after handling infected materials. Food poisoning, conversely, most often spreads through ingesting contaminated food or beverages, with less risk of person-to-person transmission unless the pathogen is viral (e.g., norovirus).
Understanding transmission risk shapes not only home hygiene but also when, how, and who you warn during illness. Reporting a suspected outbreak at a restaurant, preventing contaminated food sharing within families, and upholding rigorous handwashing in households with young children are critical steps. In healthcare settings, infection precautions are enforced for both to prevent wider community outbreaks—reinforcing the need to recognize these key differences for anyone seeking to prevent food poisoning or minimize stomach bugs among loved ones.
Stomach Bug (Viral Gastroenteritis): Spreads quickly via person-to-person contact, droplets from vomit, contaminated surfaces, and rarely contaminated food or water.
Food Poisoning: Most often contracted by consuming contaminated food or water. Rarely spreads person-to-person unless caused by a contagious virus.
Risk Groups: Who’s More Susceptible to Stomach Bug or Food Poisoning Complications?
Anyone can contract stomach flu or food poisoning, but certain risk groups face more severe complications due to their vulnerability. Young children, elderly adults, pregnant women, and individuals with weakened immune systems often experience more severe or prolonged symptoms, and face higher risk of dehydration, hospitalization, and complications from both conditions.
People with chronic illnesses (e.g., diabetes, kidney disease, heart conditions) may also have a harder time recovering and are more vulnerable to fluid loss and systemic infections. Recognizing and protecting these at-risk groups is a cornerstone of every family medicine and primary care plan.
Proactive prevention and early intervention are key for these people. Symptoms escalate more quickly, and prompt hydration, medical evaluation, and monitoring for red flag symptoms like prolonged vomiting, high fever, or confusion are essential. As infectious disease specialist Dr. Samuel Green notes:
"Young children and older adults are at higher risk for complications from both stomach bugs and food poisoning, making prompt recognition essential." — Dr. Samuel Green, Infectious Disease Specialist

What Happens First? Symptoms of Food Poisoning vs. The Start of a Stomach Bug
Recognizing the first symptoms can be pivotal for guiding your recovery or knowing when to seek help. For food poisoning, the beginning is often abrupt and severe, typically starting 1-6 hours after eating tainted food. The first signals are usually nausea, vomiting, and crampy abdominal pain, sometimes accompanied by diarrhea and even fever with food poisoning. Visual cues like pale, clammy skin or profuse sweating may also appear in severe toxin cases.
For stomach bugs, onset is typically more gradual—fatigue or mild discomfort may precede symptoms for several hours before the classic wave of nausea, vomiting, or watery diarrhea sets in. The beginning can be subtle and often confused with stress, diet, or other minor illnesses, only becoming clear as symptoms evolve.
Recording when and how your symptoms emerged compared to recent exposures (meals, sick contacts, travel) is a powerful diagnostic tool recommended by primary care and urgent care providers. This real-time tracking is one reason the “timeline test” is so valuable in clinical and home settings—helping limit spread and speeding effective recovery interventions.
What Does the Beginning of a Stomach Bug Feel Like?
The stomach bug—also known as viral gastroenteritis—often starts sneakily, with vague sensations that can be easy to dismiss. Early on, you might experience mild fatigue, a headache, or slight chills. Over the next several hours, this can build into noticeable abdominal discomfort and mild cramping. Gradually, nausea sets in, sometimes followed by vomiting and finally diarrhea.
Some people report body aches or loss of appetite in these very first stages. The overall pattern is a slow build—from feeling “not quite right” to more obvious gastrointestinal symptoms, usually within 12 to 48 hours after being exposed to someone sick or a contaminated environment.
This gradual escalation makes it easy to mix up a stomach bug with stress, dehydration, or dietary issues at first, but a distinctive pattern soon emerges: nausea and vomiting often peak first, followed by multiple episodes of watery diarrhea. Knowing these typical early sensations—and their timing—empowers you to start self-care strategies early and avoid unintentionally spreading illness to others.
What Are the First Signs of Food Poisoning?
Food poisoning has a reputation for striking fast—and hard. The very first signs often include sudden, intense abdominal pain and cramping, sometimes with overwhelming nausea that develops 1-6 hours after a risky meal. Vomiting often starts shortly after, followed by diarrhea that can sometimes be bloody, especially with severe bacterial cases like E. coli. Many affected individuals describe a rapid shift from feeling fine to violently unwell within a very short span of time. Occasionally, other symptoms such as chills, fever, or muscle aches accompany the gastrointestinal distress.
Because the symptoms emerge so quickly, they are easily linked to a particular food or drink. Severe or rapidly escalating symptoms—such as repeated vomiting, severe abdominal pain, confusion, or high fever—are recognized as “red flags” and prompt urgent consultation with a healthcare provider, especially among vulnerable groups.
How to Respond: Home Remedies and Recovery for Stomach Bug or Food Poisoning
Whether facing stomach flu or food poisoning, evidence-based home remedies and supportive care can promote faster recovery and reduce symptom severity. The cornerstone of therapy for both is hydration: replacing lost fluids and electrolytes is critical to avoid dehydration. Clear fluids—such as water, oral rehydration solutions (ORS), broths, or diluted sports drinks—should be consumed in small, frequent sips. Solid foods can be reintroduced with bland options (crackers, toast, rice, bananas) as your symptoms improve, but never force eating if nausea remains strong.
Gentle rest, avoiding caffeine and alcohol, and washing your hands frequently also speed recovery and help prevent spread. Over-the-counter medications may help with fever or aches, but anti-diarrheal drugs should only be considered with input from your healthcare provider, especially in cases suspected to involve bacterial or toxin-mediated food poisoning. Serious symptoms such as inability to keep liquids down, blood in vomit or stool, or persistent high fever require medical evaluation. As Dr. Aisha Patel, Registered Dietitian and Gut Health Specialist, says:
"Hydration is the cornerstone of recovery—drink small amounts frequently, even if you can’t keep food down." — Dr. Aisha Patel, Registered Dietitian and Gut Health Specialist
Drink plenty of clear fluids (water, diluted rehydration drinks, broth, or herbal teas)
Start with bland foods when ready (bananas, rice, applesauce, toast—BRAT diet)
Rest as much as possible and avoid strenuous activity
Wash your hands frequently and disinfect contaminated surfaces
Do not take anti-diarrheal medications unless directed by your provider
Monitor for red flag symptoms: blood in stool, dehydration, confusion, high fever
Flushing Out a Stomach Bug: Effective Steps for a Speedy Recovery
A “stomach bug” can zap energy and leave you feeling drained, but several strategies can support your body’s healing. Focus on staying well-hydrated—frequent sips of water or an electrolyte solution can prevent complications like kidney injury. Small, frequent snacks are easier to tolerate than large meals; the BRAT diet (bananas, rice, applesauce, toast) is a gentle starting point.
Allowing your digestive system rest—avoiding spicy, fatty, or dairy-heavy foods—can reduce irritation. Good hygiene is essential to prevent the spread of infection, especially in shared living spaces. Should symptoms last more than a few days, or if there is blood in the stool, severe pain, or persistent vomiting, consult your healthcare provider without delay. With patience, gentle care, and close attention to warning signs, most people rebound within a week or less.
Psychological support is also important: reassure loved ones, avoid unnecessary worry, and keep communication with primary care open—especially for high-risk individuals. Timely action can prevent food poisoning or stomach bugs from becoming more severe, and quick response is vital in fragile populations such as children, the elderly, or those with chronic illnesses.

When to See a Doctor: Red Flags That It's More Than a Simple Stomach Bug or Food Poisoning
While most cases resolve at home, certain symptoms demand urgent medical attention to prevent life-threatening complications. Persistent vomiting, inability to keep fluids down, blood in stool or vomit, confusion, rapid heartbeat, and signs of severe dehydration (such as dry mouth, sunken eyes, low urine output) are all red flags.
High fever (over 102°F/39°C)—especially coupled with chills, confusion, or persistent abdominal pain—is always a reason to consult primary care or seek urgent care without delay. Waiting too long can risk serious complications, especially in infants, elderly, and people with weakened immune systems. Keep a symptom diary and bring it to your appointment to aid rapid diagnosis and expedite treatment.
Red Flag Symptoms: When to Seek Medical Attention
Symptom |
Why It’s Dangerous |
What to Do |
|---|---|---|
Blood in stool or vomit |
May indicate severe infection, internal bleeding, or toxic bacteria |
Seek urgent care or go to the ER immediately |
Persistent vomiting or inability to keep fluids down (over 8 hours) |
Risk of severe dehydration and organ damage |
Contact healthcare provider promptly |
Signs of severe dehydration (dry mouth, no tears/urine, sunken eyes) |
May lead to kidney failure, seizures, or shock |
Immediate rehydration and urgent care visit |
High fever (>102°F/39°C) or confusion |
Possible widespread infection, sepsis, or neurological complications |
Seek emergency medical evaluation |
Symptoms last more than 3 days or worsen after 24 hours |
Risk of underlying condition or secondary infection |
Consult primary care or urgent care |

Frequently Asked Questions: Stomach Bug or Food Poisoning
How do I know if I have food poisoning or a stomach bug?
Answer: Distinguishing Between Food Poisoning and Stomach Bug Based on Symptoms and Timeline
Food poisoning often presents fast—within hours of eating contaminated food—with sudden symptoms like intense abdominal pain, vomiting, and sometimes diarrhea. A stomach bug (stomach flu/viral gastroenteritis) usually starts gradually, a day or more after contact with someone sick or contaminated surfaces, and brings milder early symptoms such as fatigue, low-grade fever, and evolving gastrointestinal upset. The timeline from exposure to illness and the context of recent risky foods or sick contact helps tell them apart.
What are the first signs of food poisoning?
Answer: Recognizing the Onset and Hallmark Symptoms of Food Poisoning
The first signs of food poisoning are often abrupt and severe. Most people experience sudden stomach cramps, nausea, vomiting, and diarrhea, typically within 1–6 hours after consuming bad food or drink. These may be accompanied by chills, sweating, and sometimes fever or muscle aches, depending on the type of pathogen involved. Keep track of what you ate prior to symptoms and seek help if signs worsen.
What does the beginning of a stomach bug feel like?
Answer: Typical Early Sensations and Symptoms of a Stomach Bug
The start of a stomach bug usually includes mild malaise, slight fatigue, a headache, or mild abdominal discomfort. These symptoms gradually intensify over several hours, leading to nausea, vomiting, and watery diarrhea. It’s common to feel “off” before gastrointestinal issues begin, which is different from the rapid onset of food poisoning.
How to flush out a stomach bug?
Answer: Safe and Effective Ways to Flush Out a Stomach Bug
Stay well-hydrated with water, broths, or oral rehydration solutions, and rest as much as possible. Start bland foods when nausea subsides and avoid dairy or greasy meals. Clean shared surfaces, wash hands regularly, and avoid anti-diarrheal medications unless approved by your provider. These steps help your body recover naturally and limit the spread of germs.
Key Takeaways: The Timeline Test for Stomach Bug or Food Poisoning
The timeline of symptoms—when they start after exposure—remains the most reliable at-home clue for distinguishing between food poisoning and a stomach bug. Early, severe symptoms after a risky meal mean food poisoning is likely; gradual onset after sick contact points to a stomach bug. Careful tracking, hydration, and attention to red flags are critical for a safe recovery.
References: Sources, Case Studies, and Expert Insights for Stomach Bug or Food Poisoning
Taking Control: Next Steps for Your Stomach Health
Trust your body’s signals: track exposures, hydrate, watch for warning signs, and never hesitate to seek help if you or a loved one is at higher risk. Empowered with this knowledge, you can recover with confidence and prevent future stomach woes. Stay informed, stay safe—and share this guide with those you care about!
If you’re interested in expanding your understanding of digestive health and want to take a more proactive approach to gut wellness, consider learning about other common gastrointestinal conditions and their prevention.
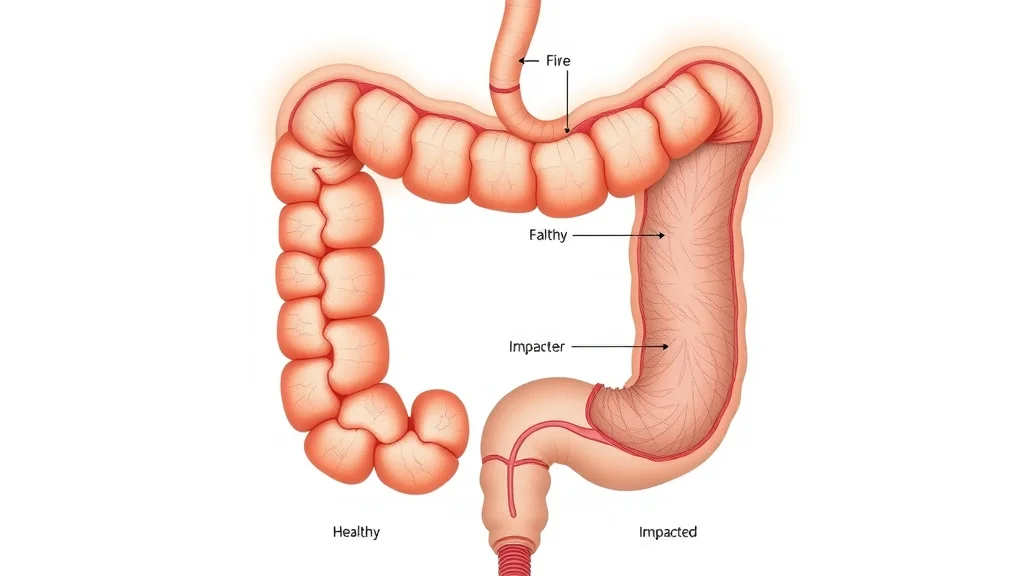
For instance, diverticulitis is another digestive issue that can cause abdominal pain and discomfort, but with different causes and risk factors than stomach bugs or food poisoning.
To gain essential insights on prevention, symptoms, and when to seek surgical advice, explore this in-depth guide to diverticulitis from leading surgeons. Building a broader knowledge base empowers you to make informed choices for your long-term digestive health.
Understanding the differences between a stomach bug (viral gastroenteritis) and food poisoning is crucial for effective management and recovery. Both conditions share similar symptoms, such as nausea, vomiting, diarrhea, and abdominal cramps, making it challenging to distinguish between them. However, the onset and duration of symptoms can provide valuable clues.
Onset of Symptoms:
Food Poisoning: Symptoms often appear rapidly, typically within 2 to 6 hours after consuming contaminated food. This quick onset is due to the body’s immediate reaction to toxins or pathogens present in the food. (healthline.com)
Stomach Bug: Symptoms usually develop more gradually, appearing 12 to 48 hours after exposure to the virus. This delayed onset reflects the incubation period of the virus as it multiplies in the body. (healthline.com)
Duration of Illness:
Food Poisoning: The illness is generally short-lived, with symptoms resolving within 1 to 3 days. The exact duration can vary depending on the specific pathogen involved. (healthline.com)
Stomach Bug: Symptoms can last from 1 to 4 days, and in some cases, up to a week. The duration depends on the specific virus causing the infection. (healthline.com)
Key Differences:
Cause: Food poisoning is caused by consuming food contaminated with bacteria, viruses, or parasites. In contrast, a stomach bug is typically caused by viruses like norovirus or rotavirus, which are highly contagious and spread through person-to-person contact or contaminated surfaces. (healthline.com)
Contagiousness: Stomach bugs are highly contagious and can spread rapidly in communities. Food poisoning, however, is usually not contagious unless caused by certain pathogens that can be transmitted from person to person. (healthline.com)
When to Seek Medical Attention:
While both conditions often resolve on their own, it’s important to seek medical care if you experience:
Severe dehydration (e.g., dry mouth, dizziness, decreased urination)
High fever (above 102°F or 39°C)
Blood in vomit or stool
Symptoms persisting longer than 3 days
Understanding these distinctions can help you manage your symptoms more effectively and prevent the spread of illness to others. NCWellnessHub.com
 Add Row
Add Row  Add
Add 


Write A Comment