Over 34 million Americans live with diabetes, yet early signs often go unnoticed. Understanding the truth behind a type 2 diabetes diagnosis can empower you to take control before complications arise. Discover what your doctor might be missing and why your knowledge matters more than ever.

The Urgency of Understanding Type 2 Diabetes Diagnosis
A type 2 diabetes diagnosis can change your life—but the real danger lies in what you might not be told during a routine checkup. Blood sugar and plasma glucose tests are only part of the puzzle. Many health care professionals focus on standard readings, but miss subtle warning signs and risk factors that could make a vital difference in early detection. With the number of people at risk climbing rapidly in the United States, urgent awareness is crucial, not just to prevent complications like vascular disease and kidney disease but to protect your overall well-being. If you know how to recognize early symptoms and key risk factors, you’re already ahead in the fight against developing type 2 diabetes.
“Type 2 diabetes is manageable, and it’s certainly not a death sentence. As long as you pay attention to it and make consistent changes—like keeping up with a healthier diet, regular checkups, and daily activity—you can live a full, normal life.” — Dr. John Anderson, Endocrinologist,
In this comprehensive guide, we dig deep into what happens during a type 2 diabetes diagnosis, why certain risk factors and signs are often overlooked, and how you can advocate for yourself. Let’s uncover what current diagnostic criteria may miss—and what that means for your health care journey. By understanding the complete picture, you will be prepared to ask your provider the right questions and catch potential issues before they become severe.

Why Early Detection of Type 2 Diabetes Diagnosis Matters
Catching type 2 diabetes early can prevent lifelong health issues. When blood sugar levels stay elevated, even slightly, your body quietly endures stress that may eventually result in serious complications—ranging from cardiovascular disease to vision loss and nerve damage. The unfortunate reality is that most cases of type 2 diabetes develop over several years, with symptoms so mild that many people don’t realize something is wrong until the damage is done. This is why early screening and understanding the nuances of plasma glucose and other diagnostic tools are essential.
Health care systems emphasize fasting plasma glucose and A1C readings, yet these aren’t always sensitive enough to detect the earliest phases of the disease. People with risk factors like a family history of diabetes or a sedentary lifestyle are at higher risk of developing type 2 diabetes sooner than expected. If caught early, lifestyle changes—such as increased physical activity, weight loss, and dietary modifications—can significantly delay or even prevent full onset. Knowing the details of oral glucose tolerance tests or how average blood sugar is measured empowers you to be proactive. Early awareness leads to action, and action leads to better outcomes.
How Subtle Warning Signs of Type 2 Diabetes Go Unnoticed
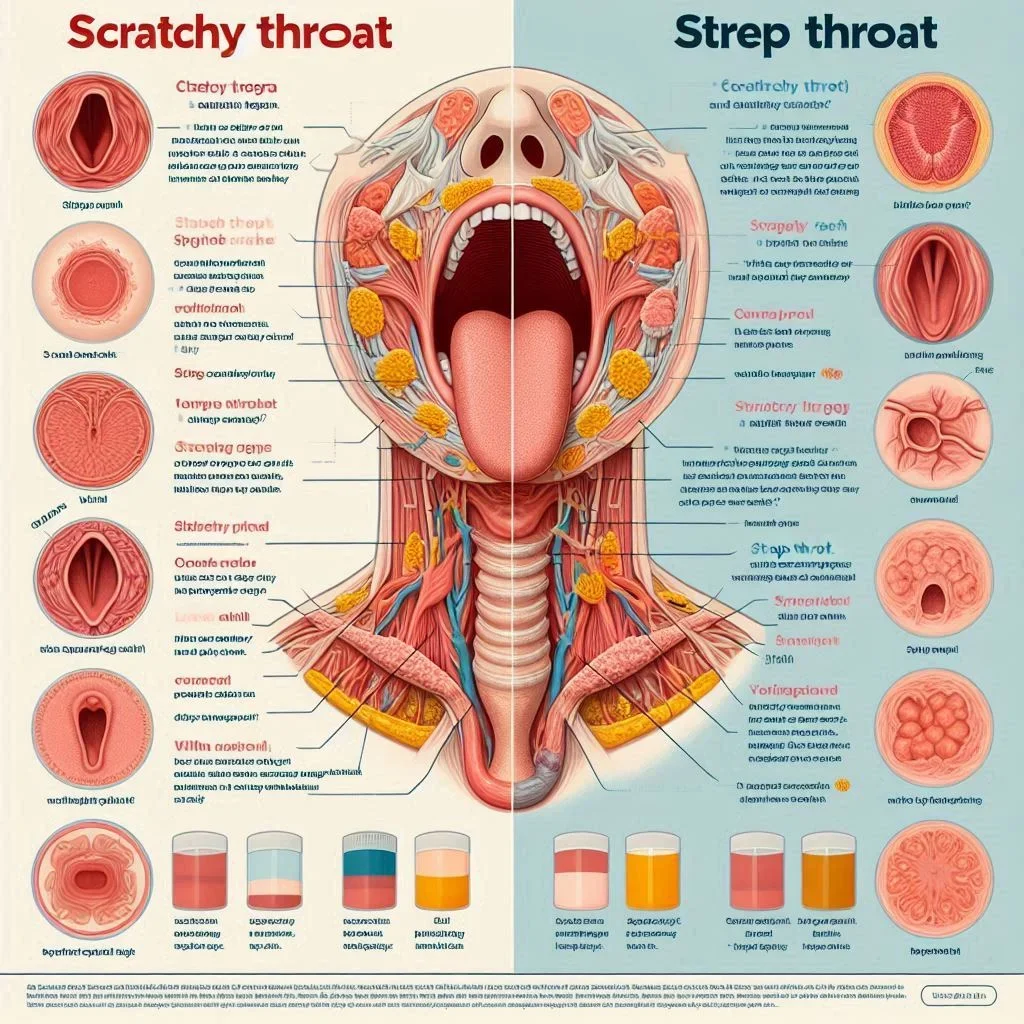
Subtle signs often fly under the radar both for patients and their health care teams. Increased thirst, frequent urination, slight fatigue, and unexpected weight loss may seem unrelated at first—yet they’re classic warning signals of rising blood glucose levels. Many patients chalk up these symptoms to stress or age, not realizing they’re the body’s alarm bells signalling insulin resistance and a possible type 2 diabetes diagnosis. Often, doctors prioritize more obvious symptoms or high-risk cases while missing critical, quiet clues in average patients.
Additionally, social factors such as ethnic background and family history, while acknowledged broadly, might not get the attention they deserve. Certain groups in the United States have a higher risk—yet screening protocols may not be as aggressive as needed. Those with prediabetes or a history of gestational diabetes are also at greater risk, but if these are not fully disclosed or discussed, a diagnosis is missed. If you notice even minor symptoms or know you have several risk factors, insist on further evaluation. Better safe than sorry when it comes to your long-term health.
“When someone is diagnosed with diabetes, it’s not about punishment or failure—it’s about partnership. Small, sustainable changes to eating habits, exercise routines, and stress management can transform health outcomes when done with guidance and patience.” — Dr. Sarah Echols, Emory Healthcare
What You'll Learn About Type 2 Diabetes Diagnosis
Key risk factors and how they impact your health
Blood sugar testing methods explained
How to interpret plasma glucose levels
What current diagnostic criteria may overlook

Breaking Down the Process: How Type 2 Diabetes Diagnosis Works
Understanding how a type 2 diabetes diagnosis is made can help you recognize what steps are standard and what questions you might need to ask. The process generally starts with an evaluation of symptoms and a look at past and present health care records, followed by specific blood sugar tests. These tests include fasting plasma glucose, the oral glucose tolerance test, and the A1C test. Health care professionals may use one or a combination of these to form their diagnosis, but knowing how each works and their potential pitfalls helps ensure you are thoroughly evaluated.
By breaking down these diagnostic steps, you can be more confident during your appointment and push for the most comprehensive evaluation possible. That includes knowing whether your health care provider has selected the best test for your risk profile, and whether additional factors—such as previous occurrences of gestational diabetes or a family history of diabetes—have been considered. Let’s explore what really happens at each phase of a type 2 diabetes diagnosis.
Health Care Professionals’ Approach to Type 2 Diabetes Diagnosis
Initially, health care professionals look for both obvious and subtle signs: unexplained fatigue, dry mouth, persistent thirst, or frequent infections can all point towards high blood sugar levels. They’ll also ask detailed questions about family history and personal habits, since risk factors like lack of physical activity, obesity, or a history of gestational diabetes significantly affect the likelihood of developing type 2 diabetes. After reviewing this information, your provider will select the most appropriate initial blood tests.
Many doctors stick with the basics—often only ordering a fasting plasma glucose test or an A1C reading. While these are excellent starting points for measuring average blood sugar and plasma glucose levels, they’re not foolproof. Because early-stage diabetes and even prediabetes can slip by with borderline results, best practice involves confirming with further testing, especially if risk factors are present. Ask your provider to explain every result and advocate for thorough screening if you have any doubts.

Blood Sugar Testing: The First Step in the Diagnosis
The cornerstone of a type 2 diabetes diagnosis is the precise measurement of blood sugar and blood glucose levels, most accurately assessed via standardized laboratory tests. The process begins with either a fasting plasma glucose (FPG) test or a random blood sugar check. The FPG test requires you to fast for at least eight hours; anything above 126 mg/dL is considered a strong indicator for a diabetes diagnosis. Blood sugar levels are measured in milligrams per deciliter and give your health care provider a snapshot of your body’s glucose handling efficiency at rest.
However, blood sugar readings can be influenced by factors such as stress, recent illness, or even temporary dietary changes. Therefore, it is crucial to follow up on borderline or abnormal results with additional testing—such as the A1C or the oral glucose tolerance test. If you are asked to repeat tests or try different methods, it’s not merely a formality, but a way to ensure accuracy and avoid false negatives that could delay much-needed treatment.
Since lifestyle changes play a pivotal role in both prevention and management, understanding how your daily nutrition impacts blood sugar is essential. For practical guidance on meal planning and making informed food choices, explore these top tips for what to eat on a low-carb diet for weight loss, which can support healthier glucose levels and overall metabolic health.
Understanding Fasting Plasma Glucose in Type 2 Diabetes Diagnosis
The fasting plasma glucose (FPG) test is central for every type 2 diabetes diagnosis. This straightforward procedure measures your blood sugar after you haven’t eaten overnight, revealing how well your body regulates glucose without the influence of recent meals. It’s one of the key criteria—levels of 126 mg/dL or higher on two separate tests typically confirm diabetes. FPG is often the first line of investigation for patients showing symptoms or those with significant risk factors, such as a family history of diabetes or obesity.
What many people don’t realize is that FPG can sometimes miss early disease. That’s why health care professionals may want to check your A1C or order an oral glucose tolerance test for a more nuanced picture. If you’re in a higher risk group—based on age, ethnicity, or past history of gestational diabetes—ask your provider if an FPG result alone is sufficient. Double-checking with additional measures ensures you won’t slip through the cracks of a basic diabetes screening.
What is the Oral Glucose Tolerance Test?
The oral glucose tolerance test (OGTT) is a powerful tool in the type 2 diabetes diagnostic arsenal, often used when initial results from FPG or A1C aren’t conclusive, or when specific risk factors raise suspicion. In this test, you’ll fast overnight and then drink a specific glucose solution shortly after arriving at the clinic. Blood samples are drawn at set intervals—usually at one-hour and two-hour marks—to see how efficiently your body clears glucose from your bloodstream. A two-hour plasma glucose reading of 200 mg/dL or more typically indicates diabetes.
The OGTT can uncover blood sugar regulation issues that might not show up in fasting tests, especially in those with prediabetes, a history of gestational diabetes, or certain ethnic backgrounds at higher risk. Because the test simulates a metabolic “stress test,” it often reveals glucose handling problems earlier in the disease process. If you’re concerned you may be at higher risk, ask your doctor about the suitability of the OGTT for your diagnosis, especially if initial tests are borderline or if you experience subtle but persistent symptoms.

The Role of A1C in Type 2 Diabetes Diagnosis
The A1C test is a measure of your average blood sugar levels over the past two to three months, providing a long-term glimpse into how well your body processes glucose. An A1C of 6.5% or higher on two separate occasions generally confirms a type 2 diabetes diagnosis. Unlike fasting or tolerance tests, the A1C doesn’t require special preparation, offering an advantage in screening large groups or individuals with unpredictable eating patterns.
A1C has limitations, however. It may not pick up short-term spikes or drops in blood sugar, and certain conditions—like anemia or kidney disease—can affect its accuracy. That’s why it’s crucial to use A1C in tandem with other diagnostic tools, especially when risk factors or subtle symptoms persist. If your result hovers near the diagnostic threshold, don’t hesitate to ask about adding further testing, like the oral glucose tolerance test or repeating the fasting plasma glucose test, for confirmation.
Who is at Risk? Unpacking Risk Factors in Type 2 Diabetes Diagnosis
Knowing your risk factors is the first step in protecting yourself from developing type 2 diabetes. While genetics and family history play a leading role, lifestyle choices and environmental factors are equally important. Common risk factors include a sedentary lifestyle, obesity, age over 45, certain ethnic backgrounds, and a history of gestational diabetes. The more risk factors you have, the higher your likelihood of developing type 2 diabetes—often earlier than you might expect.
Unfortunately, not all doctors have the time or resources to delve deeply into every patient’s full health story, sometimes missing crucial connections between everyday lifestyle and type 2 diabetes risk. Be vigilant in discussing your physical activity levels, nutrition, weight changes, and any previous diagnosis of prediabetes or other metabolic conditions. Comprehensive risk assessment is a team effort, and your input is critical to ensure a proper and timely evaluation.
Common Risk Factors Linked to Type 2 Diabetes Diagnosis
Family history of diabetes
Sedentary lifestyle
Obesity
Age and ethnic background
Anyone with a parent or sibling living with diabetes is at a significantly higher risk for developing type 2 diabetes themselves. A lack of regular physical activity and being overweight amplify this risk dramatically, especially when combined with advancing age. Certain populations—including African American, Hispanic, Asian, and Native American groups—face higher average risks for both prediabetes and type 2 diabetes, making screening and early intervention even more critical.
It’s essential to consider these broader risk factors in tandem, as many patients have more than one. For example, a middle-aged individual with a sedentary job and a family history of diabetes who also experienced gestational diabetes is at especially high risk. Don’t rely solely on your provider to connect all the dots—bring up your personal and family risk factors during every health care visit to advocate for early and comprehensive testing.

Hidden and Overlooked Risk Factor – What Your Doctor Might Miss
While traditional risk factors such as high BMI and family history get plenty of attention, one frequently overlooked contributor is the impact of stress and poor sleep. Chronic stress affects hormone levels—like cortisol—that in turn increase insulin resistance and lead to elevated blood sugar levels. Similarly, poor sleep or untreated sleep apnea is linked to higher risk of developing type 2 diabetes, a fact not always discussed in a routine appointment.
Environmental exposures, such as certain medications or long-term exposure to specific chemicals, can also heighten your risk, yet these tend to be underreported or misunderstood. If you feel your lifestyle is healthy but you’re seeing unexplained symptoms or have a strong family history, ask about these lesser-known influences. By taking a proactive approach and asking tough questions, you can help ensure nothing slips through the cracks on your path to getting, or preventing, a type 2 diabetes diagnosis.
The Interplay Between Prediabetes, Gestational Diabetes, and Type 2 Diabetes Diagnosis
Prediabetes is a state where blood sugar levels are higher than normal but not high enough to be called diabetes—yet this condition puts you at serious risk for developing type 2 diabetes. Those with a history of gestational diabetes (diabetes during pregnancy) are also at higher risk for progression to type 2 diabetes in later life, regardless of age or other traditional risk factors.
If you've ever been told you have prediabetes or had gestational diabetes during a pregnancy, it is vital to get regular screenings and consider lifestyle strategies to lower your risk. Doctors sometimes overlook this connection, so always mention these conditions during checkups or when discussing symptoms. Quick detection of rising blood glucose levels in these groups can make the difference between managing your risk and facing life-altering complications.
Tests Involved in Type 2 Diabetes Diagnosis: Beyond the Basics
Accurate identification relies on a mix of well-established and more detailed blood tests. While standard screenings like fasting plasma glucose and the A1C are widely used, secondary steps—such as the oral glucose tolerance test or more advanced plasma glucose measurements—offer a clearer clinical picture. Let’s look at what these tests actually measure, when they’re most useful, and how common pitfalls can affect your results.
Understanding the complete range of testing allows you to better interpret your results, ask for appropriate follow-ups, and avoid the distress of false negatives or delayed diagnosis. Knowledge empowers you to insist on thoroughness and accuracy in partnership with your health care team.
In-Depth Look at Plasma Glucose Measurements
Plasma glucose measurements—whether from fasting, random, or timed draws—represent the “gold standard” for pinpointing blood sugar abnormalities. Fasting plasma glucose offers a snapshot after at least eight hours without food, while random draws help capture fluctuations throughout the day. These readings, taken together, help health care providers assess both the magnitude and persistence of elevated blood glucose, which is essential for confirming a type 2 diabetes diagnosis.
Because blood sugar can be affected by factors like stress, illness, or medications, it’s often best to repeat abnormal results and confirm with secondary tests. Your provider may also use these numbers in conjunction with A1C and OGTT to check for hidden disease, especially if you have multiple or subtle symptoms. Always request explanations for your test results, so you can track progress or catch changes early.
Oral Glucose Tolerance and Tolerance Test Procedures
The oral glucose tolerance test is not just for initial diagnosis—it is sometimes repeated over time to monitor patients at higher risk or with borderline results. The procedure requires fasting beforehand, measurement of baseline plasma glucose, consumption of a set dose of glucose, and then scheduled blood draws to track the body’s handling of sugar. Elevated readings at the one or two-hour marks indicate impaired glucose tolerance or outright diabetes.
This test is particularly valuable in uncovering glucose tolerance issues in people with normal fasting glucose but elevated post-meal spikes—an early sign of diabetes missed by simple fasting tests. If your readings are close to the cutoffs for diagnosis, or you have multiple risk factors, requesting an OGTT can help protect you from an overlooked or late diagnosis.
Glucose Tolerance Test vs. Oral Glucose Tolerance Test: Key Differences
The terms “glucose tolerance test” and “oral glucose tolerance test” are sometimes used interchangeably, but the “oral” test specifically involves drinking a glucose solution, while general “tolerance” measures may include other glucose-loading strategies. The OGTT is the standard for diagnosing type 2 diabetes, as endorsed by leading diabetes organizations.
Some clinics offer additional glucose challenge tests for purposes like gestational diabetes screening or to check specific insulin resistance patterns. If in doubt, ask your health care provider exactly which test is being ordered and how it fits into the broader assessment plan for your blood sugar and plasma glucose levels.
Comparison of Common Diagnostic Tests for Type 2 Diabetes
Test |
Measures |
Key Threshold |
Pros |
Cons |
|---|---|---|---|---|
Fasting Plasma Glucose (FPG) |
Blood Sugar after fasting 8 hours |
≥126 mg/dL (diabetes) |
Simple, low cost |
May miss early disease |
Oral Glucose Tolerance Test (OGTT) |
Blood Sugar before & 2 hrs after glucose drink |
≥200 mg/dL (2-hr, diabetes) |
Detects subtle issues |
Time-consuming, prep required |
A1C |
Average blood sugar (2–3 months) |
≥6.5% (diabetes) |
No fasting needed |
Some conditions affect results |

False Negatives and Diagnostic Pitfalls in Type 2 Diabetes Detection
Even well-established blood sugar tests can miss cases of type 2 diabetes, especially in early or borderline situations. False negatives may occur if you’re tested during a time of low stress, recent illness, or after dramatic changes in routine. Some people have glucose levels that fluctuate widely, which means a single test may not tell the full story. Patients relying on minimal symptom reporting or quick screening could easily be underdiagnosed, especially if underlying risk factors aren’t fully explored.
To ensure you receive the most accurate diagnosis, always follow pre-test instructions precisely and ask about repeating questionable or marginal results. If you have ongoing symptoms, a strong family history of diabetes, or conditions like prediabetes and gestational diabetes in your background, request further testing beyond what’s typical. Thoroughness now avoids missed diagnoses and protects your long-term health.
"Many cases of type 2 diabetes remain undiagnosed for years—understanding diagnostic nuances could save lives." – Endocrinology Specialist
People Also Ask About Type 2 Diabetes Diagnosis
What are the first warning signs of type 2 diabetes?
Early symptoms are often subtle but can include increased thirst, frequent urination, and unexplained fatigue. These arise due to elevated blood sugar and blood glucose levels as the body struggles with insulin resistance. Some people may also notice mild weight loss or blurry vision. If you or someone you know experiences even one of these symptoms, requesting a type 2 diabetes diagnosis evaluation is wise. The sooner high glucose is recognized, the greater the chance to reverse damage and prevent future complications.

How do you confirm if you have type 2 diabetes?
Confirmation requires medical evaluation using standardized tests: the fasting plasma glucose test, A1C, and the oral glucose tolerance test. These measure your blood’s handling of sugar in both normal and stressed conditions. Diagnosis is confirmed if any of these tests meet or exceed the criteria for diabetes, typically after repeat measurements. It is important that all testing and interpretation be handled by an experienced health care provider to ensure reliability and safety.
What is a diabetic seizure?
A diabetic seizure happens when blood sugar drops to dangerously low levels (severe hypoglycemia). This condition isn’t as directly linked to a type 2 diabetes diagnosis as high blood sugar is but can be a risk, especially in those on certain diabetes medications. Recognizing and addressing risk factors for wildly fluctuating sugar is an essential part of managing and diagnosing all forms of diabetes. If you have type 2 diabetes or prediabetes, understanding both high and low blood sugar complications is crucial.
“Be patient with yourself. There’s a lot to learn, and it’s overwhelming at first, but over time managing diabetes becomes second nature. Each small step toward healthier choices makes a big difference.” — Cassie Haupt, Certified Diabetes Educator and Physician Assistant
What are the three criteria for diagnosing diabetes?
The main standards used to diagnose diabetes are: (1) a fasting plasma glucose of 126 mg/dL or higher, (2) a two-hour plasma glucose level of 200 mg/dL or more following an oral glucose tolerance test, and (3) an A1C result of 6.5% or greater. Meeting any one of these confirms a diagnosis—especially after more than one test. These benchmarks help detect diabetes early, making early intervention possible.

Frequently Asked Questions (FAQs) About Type 2 Diabetes Diagnosis
Can type 2 diabetes be misdiagnosed? Yes. While high blood sugar can be measured accurately, the type of diabetes can be misclassified. Adults are sometimes labeled with type 2 diabetes when they actually have LADA (latent autoimmune diabetes in adults), a slower-onset form of type 1 that still requires insulin as the disease progresses.
How often should I be screened for type 2 diabetes? Most adults should begin screening for type 2 diabetes at age 35 and repeat at least every 3 years if results are normal. If you have risk factors — such as being overweight or obese, a family history of diabetes, high blood pressure, abnormal cholesterol, physical inactivity, a history of cardiovascular disease, polycystic ovary syndrome (PCOS), or you belong to a higher-risk ethnicity (e.g., African American, Hispanic/Latino, Native American, Asian American, Pacific Islander) — screening should start earlier and be done more frequently, often every 1–2 years. People with prediabetes should be tested annually. Women who had gestational diabetes should be screened postpartum and then every 1–3 years lifelong.
What steps should I take after a diagnosis? Start by building a care team and getting a clear baseline. Schedule diabetes self‑management education, see a registered dietitian, and review your targets with your clinician (often A1c <7% but individualized). Get recommended screenings: blood pressure, A1c, fasting lipids, kidney function and urine albumin, liver enzymes, a dilated eye exam, foot exam, and dental check. Ask about vaccines (flu, COVID‑19, pneumococcal, hepatitis B), smoking cessation, and an initial medication plan — metformin is common unless contraindicated; GLP‑1 receptor agonists or SGLT2 inhibitors may be added, especially with heart, kidney disease, or if weight loss is a goal.
Is type 2 diabetes reversible if caught early? In many cases, type 2 diabetes can go into remission if it’s identified and treated early. Early in the disease, the pancreas often retains enough beta-cell function that reducing insulin resistance and easing glucose load can normalize blood sugars. Significant weight loss — especially reducing visceral (abdominal) fat — improves insulin sensitivity, sometimes to the point that A1C returns to non-diabetic levels without medication. Intensive lifestyle changes (a calorie-controlled, nutrient-dense diet; regular physical activity; good sleep; and stress management) are the cornerstone. Some people also benefit from medications like metformin, GLP-1 receptor agonists, or SGLT2 inhibitors, and for those with higher weights, metabolic/bariatric surgery has one of the highest remission rates. It’s important to understand that remission isn’t the same as a cure. The underlying susceptibility remains, and blood sugars can rise again if weight is regained or habits lapse, so ongoing monitoring and healthy routines are essential.
Key Takeaways for Patients Seeking a Type 2 Diabetes Diagnosis
Symptom recognition is critical
Clear understanding of blood sugar and plasma glucose tests supports better decisions
Don’t overlook risk factors—family history and lifestyle count
Insist on thorough health care evaluations
Protect Your Health: Act Early in Your Type 2 Diabetes Diagnosis Journey
By advocating for yourself, recognizing symptoms, and demanding comprehensive blood sugar testing, you lower your risk for late or missed diagnosis. Empowerment is your best protection against the silent progression of type 2 diabetes.
Final Thoughts on Empowering Yourself Beyond the Doctor’s Office
Your health care journey is a partnership. Understanding type 2 diabetes diagnosis in detail puts you in the driver’s seat—ask questions, monitor symptoms, and request the right tests. Knowledge is your greatest ally.
Take Charge: Schedule Your Type 2 Diabetes Screening with a Specialist Today
Don’t wait. If any risk factors or symptoms apply to you, reach out to a qualified health care provider and schedule a type 2 diabetes diagnosis screening now. Early detection saves lives.
As you continue your journey toward better health, remember that managing type 2 diabetes risk is about more than just numbers—it's about holistic well-being. If you’re looking to address underlying contributors like chronic stress, which can quietly impact blood sugar and overall health, consider learning simple strategies to reset your mind and body. Discover how a quick, effective stress detox can support your wellness goals by reading this guide to a 5-minute stress detox. Taking small, mindful steps today can lead to lasting improvements in your health and resilience.
Sources
Understanding the nuances of a type 2 diabetes diagnosis is crucial for early detection and effective management. The article “Type 2 Diabetes | Johns Hopkins Medicine” provides a comprehensive overview of diagnostic tests, including the A1C test, fasting plasma glucose, and oral glucose tolerance test, detailing their procedures and interpretation of results. (hopkinsmedicine.org)
Additionally, the “Diabetes Tests & Diagnosis - NIDDK” outlines who should be tested for diabetes, the specific tests used, and what the results indicate, offering valuable insights into the diagnostic process. (niddk.nih.gov) If you’re serious about understanding and managing type 2 diabetes, these resources will provide you with essential information to navigate your health journey.
 Add Row
Add Row  Add
Add 



Write A Comment