Did you know that eye floaters affect nearly everyone as they age, often signaling changes in the eye’s gel-like interior? Understanding what causes eye floaters can help you distinguish harmless spots from symptoms needing urgent care. Let’s unravel this common eye mystery together.
Understanding What Causes Eye Floaters: Quick Insights
-
What are eye floaters? Eye floaters are small, shadowy shapes that drift in your field of vision. They often look like spots, squiggly lines, or tiny cobwebs. These visual disturbances are most noticeable when looking at a bright background, such as the sky or a blank wall.
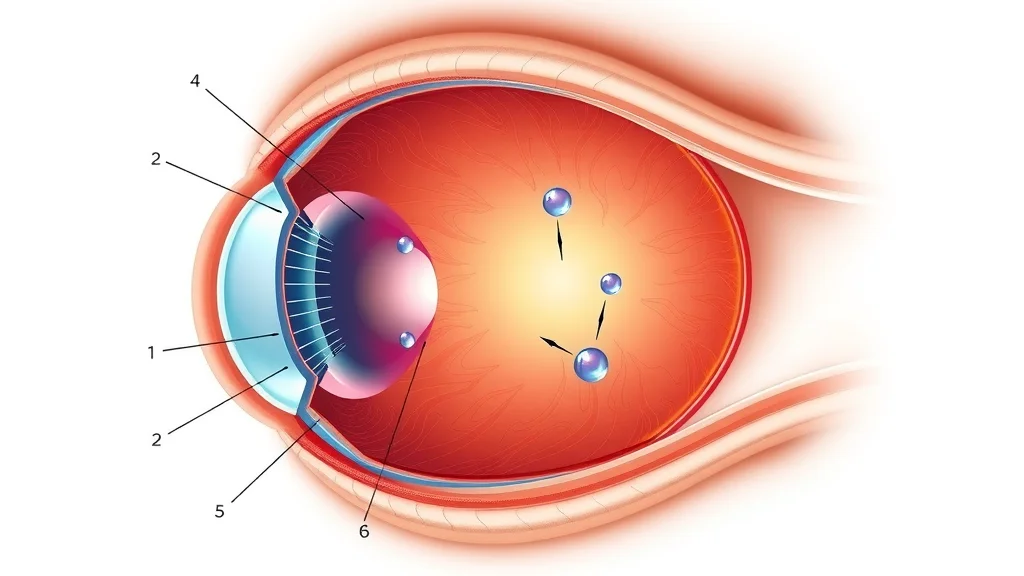
Floaters occur when tiny bits of the vitreous gel, located at the back of the eye, cast shadows on the retina. Most people experience floaters at some point, though their prevalence increases with age and specific eye conditions.

-
How do eye floaters develop? Floaters develop as the clear, gel-like vitreous inside the eye slowly changes over time. With aging, this gel can shrink and become more liquid, causing small clumps or strands that move with your eye.
As the vitreous detaches from the retina, these clumps drift, explaining why floaters seem to dart away when you try to look at them directly. Sometimes, sudden floaters result from injury, inflammation, or bleeding inside the eye, warranting immediate medical attention.
Immediate signs: Knowing 'what causes eye floaters' and 'how floaters appear' Spotting floaters can be a normal part of aging, but a sudden shower of new floaters, flashes of light, or loss of side vision may warn of more serious issues, such as retinal detachment. Recognizing these signs and knowing what causes eye floaters is crucial for taking prompt action.
What You'll Learn About What Causes Eye Floaters
Essential facts about eye floaters and their origins
Understanding links between eye health, the aging process, and floaters
Prevention and treatment options explained
When to see an eye doctor or eye health specialist
What Causes Eye Floaters: Core Mechanisms
-
The role of the vitreous gel and its aging process The center of your eye is filled with a clear, gel-like substance called the vitreous humor. As we age, this gel begins to shrink and liquefy. Tiny fibers within the vitreous can clump together, casting shadows that appear as floaters.
Posterior vitreous detachment (PVD) occurs when the shrinking gel pulls away from the retina, frequently causing an increase in floaters. This natural progression highlights aging as the key factor in what causes eye floaters.
-
Posterior vitreous detachment and the development of floaters Posterior vitreous detachment is a common age-related condition. As the vitreous separates from the retina, it leaves behind clumps and web-like strands. Floaters are created as light passes through these irregularities, casting unpredictable shadows onto your retina and manifesting as visible floaters.
While most PVD cases are harmless, some can lead to retinal tears or detachments, which are serious eye problems that require urgent care from a qualified eye doctor.
-
Aging process as a primary factor Age is the single most significant risk factor for developing eye floaters. The vitreous breakdown and gel separation accelerate after age 50, making floaters a common occurrence for older adults. Genetics, eye health history, and previous eye complications can increase susceptibility. As Dr. Alicia Warren, Ophthalmologist, notes:
"The breakdown of the vitreous gel is a natural part of aging, often leading to floaters."
While understanding the aging process and vitreous changes is essential, it's equally important to recognize the subtle warning signs that may indicate more serious eye issues. For a deeper look at symptoms you shouldn't ignore, explore the most common warning signs of eye problems that often go unnoticed but can have a significant impact on your vision.
Eye Health and Other Medical Causes Behind What Causes Eye Floaters
Eye injuries and trauma Traumatic injuries to the eye or head can cause sudden floaters by damaging retinal blood vessels or causing hemorrhage in the vitreous gel. These floaters are frequently accompanied by pain or vision changes and should prompt an immediate eye exam.
Diabetic retinopathy and bleeding inside the eye Uncontrolled diabetes can damage retinal blood vessels, leading to bleeding. Blood in the vitreous can create new, prominent floaters that persist until the blood is reabsorbed or surgically removed.
High blood pressure and its indirect relationship to floaters Chronic high blood pressure can weaken the blood vessels of the eye, leading to microbleeds into the vitreous. While less common than aging or injury, blood pressure-related floaters signal the need for a full health evaluation.
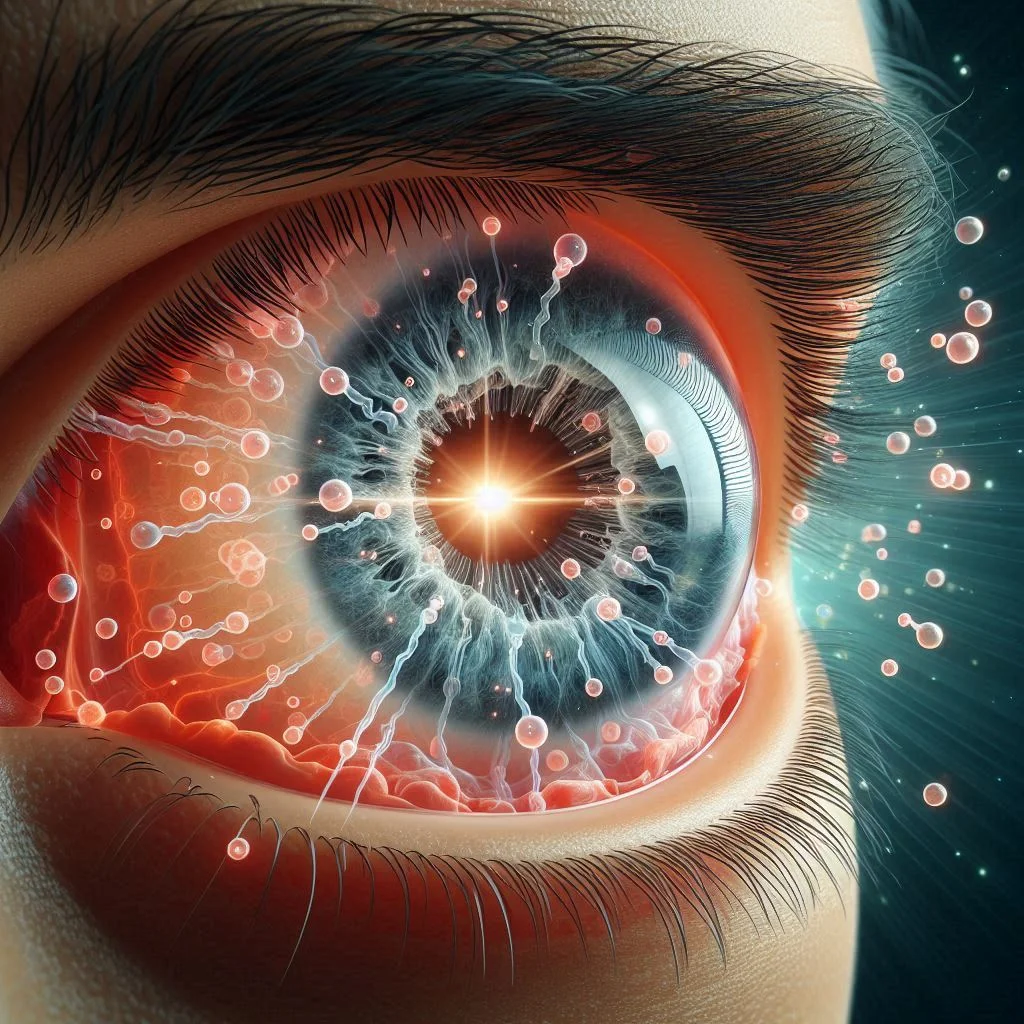
Inflammation, infection, and uveitis Certain inflammatory conditions (like uveitis) or infections can introduce cellular debris, pus, or blood into the vitreous, causing floaters and signaling possible eye infection or autoimmune response. These cases may cause associated pain, redness, or blurred vision.
-
As Dr. Samuel Lin, Retina Specialist, emphasizes:
"Some conditions like uveitis or diabetic eye disease can contribute to sudden floaters."
Sudden Floaters vs. Gradual: What Causes Each Type?
Sudden floaters and symptoms of retinal detachment Sudden onset of many new floaters, especially with flashes of light or a shadow in your side vision, can indicate a retinal tear or detachment. This is a sight-threatening emergency that requires immediate attention from an eye care provider. Sudden floaters can also signal bleeding or trauma. Early intervention can save vision in many cases.

Gradual onset: Posterior vitreous detachment and aging process When floaters appear slowly and without pain or vision changes, they are typically related to age-related vitreous changes or PVD. These floaters may remain stable or slowly increase over the years, but often aren’t dangerous.
Risk factors for each type Sudden floaters are associated with trauma, high myopia, severe diabetes, and inflammatory disorders. Gradual floaters are linked primarily to the natural aging process, genetics, and general eye health.
Table: Common Causes of Eye Floaters and Their Symptoms
Cause |
Typical Symptoms |
Urgency |
Diagnosis Path |
|---|---|---|---|
Aging Process |
Gradual onset of mild floaters; often asymptomatic beyond visual spots |
Routine evaluation if persistent |
Eye exam, dilated eye exam |
Posterior Vitreous Detachment |
Sudden increase in floaters, sometimes flashes of light |
Prompt eye doctor visit |
Dilated retinal exam, OCT |
Vitreous Hemorrhage |
Dense, sudden floaters; possible vision loss |
Emergency evaluation |
Eye doctor, retinal imaging |
Retinal Detachment |
Sudden floaters with flashes and shadow/curtain loss of vision |
Immediate emergency |
Urgent dilated exam, imaging |
Eye Injuries |
Acute floaters with pain, blurred vision |
Emergency intervention |
Physical exam, eye imaging |
Inflammation |
Floaters, redness, eye pain |
Prompt specialist review |
Eye doctor, lab tests |
High Blood Pressure |
Chronic, sometimes with other vascular symptoms |
Monitor and manage underlying cause |
Blood pressure check, eye exam |
Spotting Danger: When Are Eye Floaters a Sign of Something Serious?
Symptoms that require immediate attention: flashes, shadows, sudden increase Contact an eye doctor right away if you experience a sudden shower of floaters, bright flashes of light, visual shadows, or a sudden change in vision. These may all indicate a retinal tear, detachment, or internal bleeding.

Risk factors for retinal detachment Risk increases in those with severe nearsightedness, prior eye injuries, eye surgery, strong family history, or certain eye conditions such as lattice degeneration. These individuals should remain vigilant for sudden vision changes.
-
Expert advice: Dr. Priya Choudhury, Optometrist, urges:
"If you experience a sudden shower of new floaters or flashing lights, contact an eye doctor promptly."
How an Eye Doctor Diagnoses What Causes Eye Floaters
Routine eye exam process Diagnosis starts with a comprehensive eye exam. Your eye doctor will ask about your symptoms and medical history, then perform a thorough retinal evaluation. Eye drops are often used to dilate your pupils for a better view of the back of the eye.
Technologies: Optical coherence tomography (OCT), dilated eye exams State-of-the-art imaging like OCT, slit lamp microscopy, and fundus photography help detect subtle changes to the retina and vitreous gel. These tools are vital for identifying retinal tears, detachment, or other causes of eye floaters that may need urgent management.

Importance of medical history and symptom reporting Be honest and detailed about your symptoms, especially when they started and how rapidly they changed. This information can help pinpoint what causes your eye floaters and whether further testing or treatment is necessary.
Watch a leading ophthalmologist explain what causes eye floaters, what to watch for, and new advances in floaters management. [Insert video here]
Treatment Options: Can You Get Rid of What Causes Eye Floaters?
Observation and reassurance In most cases, floaters are harmless and require no treatment other than regular monitoring through routine eye exams. Many people find floaters become less noticeable over time as the brain adapts.

When medical or surgical intervention is warranted If floaters significantly impair vision or result from retinal detachment or hemorrhage, treatment is necessary. Eye care providers may recommend surgery or laser therapy based on individual risk factors.
Laser treatment and vitrectomy: Pros, cons, and safety YAG laser vitreolysis breaks up prominent floaters but carries a small risk of complications including retinal tears. Vitrectomy, the surgical removal of the vitreous gel, is a last resort due to potential risks (infection, cataracts) and is typically reserved for severe, persistent floaters.
New research and emerging therapies Ongoing studies are exploring safer non-surgical treatments and drugs that may dissolve floaters. Ask your eye doctor about clinical trials and the latest options.
Lifestyle and Home Management for Eye Floaters
Maintaining optimal eye health Healthy vision starts with regular eye care and monitoring. Routine eye exams allow early identification of disease and keep your eyes in top condition.
Managing high blood pressure and other risk factors Since high blood pressure, diabetes, and chronic inflammation can contribute to eye floaters, manage these conditions with the guidance of your healthcare provider.
Protecting eyes from injury Always use protective eyewear in sports or hazardous environments to lower your risk of traumatic floaters and other eye problems.

Diet and supplements that support healthy vision Eating a diet rich in leafy greens, colorful vegetables, and omega-3 fatty acids can boost retinal health. Some supplements containing antioxidants, vitamin C, and zinc support the aging process of the eye but consult your doctor first before beginning any new regimen.
Eye Floaters in One Eye vs. Both: What Causes the Difference?
Assessing asymmetry in floater symptoms Floaters appearing in just one eye often suggest an underlying localized problem, such as eye trauma, localized bleeding, or infection. When floaters occur in both eyes simultaneously, age-related changes are the most likely culprit.
Conditions more likely to cause floaters in one eye such as trauma or local bleeding Unilateral floaters (floaters in one eye) raise suspicion of acute problems including vitreous hemorrhage, inflammation (uveitis), or physical injury and always merit a thorough dilated eye exam by an eye care provider.
Prevention: Can You Lower Your Risk of What Causes Eye Floaters?
Eye health checkups and early intervention Schedule regular eye exams especially as you age or if you have risk factors like diabetes, high blood pressure, or family history of eye conditions.
Managing systemic factors like diabetes and high blood pressure Good control of blood sugar and blood pressure can reduce your risk of complications that may result in floaters or vision loss.

Eye safety practices Always wear protective eyewear during activities that could lead to eye injury and be alert to any sudden changes in your vision.
-
Key tips list for prevention
Get regular eye exams every 1–2 years
Monitor and manage blood pressure and blood sugar
Wear protective eyewear for sports or work
Eat a vision-supportive diet high in antioxidants
Don’t ignore sudden vision changes—see an eye doctor immediately
FAQs About What Causes Eye Floaters and Eye Health
Do eye floaters go away on their own? Most eye floaters become less noticeable over weeks or months as your brain learns to ignore them. Rarely, floaters vanish completely. Persistent, bothersome floaters should still be assessed by an eye doctor.
Can you prevent all types of eye floaters? It’s impossible to prevent all floaters, especially those caused by natural aging. However, controlling blood pressure, blood sugar, and protecting your eyes can limit your risk of floaters triggered by injury or disease.
Is there any risk of vision loss from eye floaters? Most floaters are harmless, but if associated with retinal tears, detachment, or bleeding, vision loss can occur unless treated promptly. Early detection is critical to preventing complications.
Will everyone experience floaters eventually? The vast majority of people notice floaters by their senior years, but not everyone will find them problematic. Those with high myopia or a history of eye problems may see them earlier.
People Also Ask: What Triggers Eye Floaters?
What triggers eye floaters?
Eye floaters are generally triggered by natural changes to the vitreous gel during the aging process, but can also be caused by injury, bleeding, inflammation, or rapid changes in eye health, such as posterior vitreous detachment or retinal detachment.
How do you get rid of eye floaters?
Many eye floaters do not require treatment and may become less noticeable over time. Interventions like laser therapy or vitrectomy are reserved for severe cases and must be evaluated by a qualified eye doctor.
When should I worry about eye floaters?
Sudden appearance of many floaters, especially with flashes of light or vision loss, can signal retinal detachment or bleeding and needs urgent medical attention.
Do floaters go away on their own?
Most floaters become less noticeable over time as the brain adapts but rarely disappear outright. If they persist, consult an eye doctor to rule out underlying issues.
Case Study: When Eye Floaters Revealed a Hidden Condition
Real patient experience involving sudden floaters A 62-year-old patient experienced a sudden burst of floaters in one eye, accompanied by brief flashes of light but no pain. Concerned, she visited her eye doctor the same day.

Step-by-step diagnostic journey The eye care provider performed a dilated eye exam and ordered an OCT scan, identifying a small retinal tear caused by posterior vitreous detachment. The tear was promptly treated with laser therapy, preventing complications.
Outcome and lessons for maintaining eye health Thanks to early action and comprehensive diagnosis, the patient’s vision was preserved, with floaters becoming less noticeable over the following months. This highlights the importance of recognizing when floaters signal a deeper issue and the value of regular eye exams.
Key Takeaways on What Causes Eye Floaters
Main causes, warning signs, and prevention methods summarized: Most floaters are a normal result of aging, but sudden changes can mean serious issues like retinal detachment, especially with flashes of light.
Importance of prompt care in high-risk cases: Seek an eye doctor’s assessment if you notice a sudden increase in floaters or experience visual disturbances.
Directing readers to reliable resources: Consult eye health professionals and visit trusted sites like NCWellnessHub.com for further information.
Conclusion: Protecting Your Vision—What to Remember About What Causes Eye Floaters
Timely action is key
Consult an eye doctor if in doubt
Commit to regular eye health checks
Explore further at NCWellnessHub.com for trusted wellness information
If you’re interested in taking your eye health knowledge even further, consider learning about advanced prevention strategies and holistic approaches to vision care. Our comprehensive guide on NAC eye drops and their potential to reverse cataracts delves into innovative treatments and proactive steps for maintaining lifelong visual wellness. Discover how staying informed about emerging therapies can empower you to make the best choices for your eyes and overall health.
Sources
Eye floaters are small, shadowy shapes that drift across your field of vision, often resembling spots, squiggly lines, or tiny cobwebs. They are most noticeable when looking at bright backgrounds, such as the sky or a blank wall. These visual disturbances occur when tiny bits of the vitreous gel inside the eye cast shadows on the retina.
While most people experience floaters at some point, their prevalence increases with age and certain eye conditions. Understanding the Causes of Eye Floaters The primary cause of eye floaters is age-related changes in the vitreous humor—the clear, gel-like substance that fills the center of the eye.
As we age, this gel begins to shrink and liquefy, leading to the formation of clumps or strands that cast shadows on the retina, perceived as floaters. This process, known as posterior vitreous detachment (PVD), is common and typically harmless. (mayoclinic.org)
However, sudden onset of numerous floaters, especially when accompanied by flashes of light or loss of peripheral vision, may indicate more serious conditions such as retinal tears or detachments. These situations require immediate medical attention to prevent potential vision loss. (nei.nih.gov)
Other Contributing Factors Beyond aging, several factors can contribute to the development of eye floaters: Eye Injuries and Trauma: Physical injury to the eye can lead to vitreous detachment or bleeding, resulting in floaters. (scripps.org) Diabetic Retinopathy: Uncontrolled diabetes can damage retinal blood vessels, leading to bleeding into the vitreous and subsequent floaters. (my.clevelandclinic.org)
Inflammation and Infections: Conditions like uveitis cause inflammation in the eye, introducing debris into the vitreous that appears as floaters. (hopkinsmedicine.org) High Blood Pressure: Chronic hypertension can weaken retinal blood vessels, leading to microbleeds that manifest as floaters. (scripps.org)
When to Seek Medical Attention While many floaters are benign, it’s crucial to recognize symptoms that warrant immediate care: A sudden increase in the number of floaters Flashes of light A shadow or curtain over part of your vision These signs could indicate retinal detachment or other serious conditions. Prompt evaluation by an eye care professional is essential to preserve vision. (mayoclinic.org)
Diagnosis and Treatment Diagnosis typically involves a comprehensive eye exam, including pupil dilation to examine the retina and vitreous. Most floaters do not require treatment and may become less noticeable over time. However, if they significantly impair vision, options like laser therapy or vitrectomy (surgical removal of the vitreous) may be considered. (mayoclinic.org)
Preventive Measures
Maintaining overall eye health can reduce the risk of floaters:
Regular eye exams
Managing chronic conditions like diabetes and hypertension
Protecting eyes from injury
Adopting a diet rich in antioxidants and omega-3 fatty acids
Understanding the causes and implications of eye floaters empowers individuals to take proactive steps in preserving their vision. For a visual explanation of what causes eye floaters, you might find this video helpful: What causes flashes and floaters?
 Add Row
Add Row  Add
Add 




Write A Comment