Ever wondered, 'Why does my knee pop?' That sudden sound can be surprising—but what does it actually mean? Understanding the causes helps you protect your joints and know when to seek help. Let's uncover the truth behind those mysterious knee pops for your health and peace of mind.

What You'll Learn in This Guide to Why Does Knee Pop?
Understand why knee pops occur
Identify common causes of knee popping and knee pain
Recognize when to see an orthopedic surgeon or knee specialist
Explore treatments and preventive strategies recommended by experts
Why Does My Knee Pop? Understanding the Sounds from Your Knee
Why the Popping Sound in Your Knee Matters
For many people, a knee pop is a daily experience—whether it’s getting out of bed in the morning or rising after sitting for a while. But what do those popping sounds really mean? Are they a harmless quirk of biology or a warning sign your body is trying to give you?
These questions are more than curiosity—knowing the difference can help you manage your joint health and take smart steps to protect your knees. By understanding when a knee popping noise is normal and when it may signal a problem, you can take charge of your wellbeing and avoid future complications.
The truth is, while most episodes of knee popping or knee clicking are benign, some sounds—especially those accompanied by pain or swelling—can indicate underlying issues like a meniscus tear, cartilage damage, or instability of the ligament or tendon around the knee joint. Recognizing the warning signs and understanding the mechanics behind the "pop" can help you know when it’s time to see an orthopedic surgeon or knee specialist, and what to expect during your evaluation. Let’s dive into why your knee pops and how you can keep your joints healthy for years to come.

Overview: What Does Knee Popping Really Mean?
Knee popping, or the sensation and sound of a "pop" in your knee, is a common occurrence and can be caused by various factors. Sometimes, these noises happen when you move your knee from a bent to a straight position or vice versa. The popping sound itself can happen due to harmless reasons—such as the release of gas bubbles in the synovial fluid or ligaments lightly sliding across a bony prominence. However, at other times, knee popping can involve structural issues inside the knee joint, such as a piece of cartilage moving out of place or a meniscus tear causing an abnormal popping sensation.
Clinically, orthopedic surgeons use the context of the pop—such as recent knee injury, the presence of knee pain, or swelling—to determine if further evaluation is needed. If popping is frequent, associated with pain or swelling, or follows trauma (like twisting during a sport), it may signal a need for medical attention to prevent long-term damage. Getting clarity on these factors helps you distinguish between normal and concerning popping, so you can protect your mobility and joint health.
How Experts Study Knee Pop Concerns
Orthopedic surgeons and knee specialists rely on decades of research, real-world case studies, and peer-reviewed evidence to determine the causes and treatment strategies for this common complaint. Physical therapists also play a vital role—studying the biomechanics of the knee joint and how factors like muscle balance, cartilage wear, or instability contribute to knee popping.
Most guidelines recommend comprehensive patient history, careful physical examination, and objective imaging (like MRI or X-rays) to distinguish minor, episodic "popping" from situations where a meniscus tear, ligament or tendon injury, or cartilage damage may be present. This evidence-based approach ensures you receive accurate diagnoses and the most effective care tailored to your unique situation.

Common Causes of Knee Popping Explained by Orthopedic Surgeons
"Many cases of knee popping are harmless, but persistent or painful popping should always be evaluated. It can signify issues ranging from cartilage damage to ligament problems." – Dr. Laura Chang, Board-Certified Orthopedic Surgeon
Why Does Knee Pop? The Roles of Gas Bubbles and Biomechanics
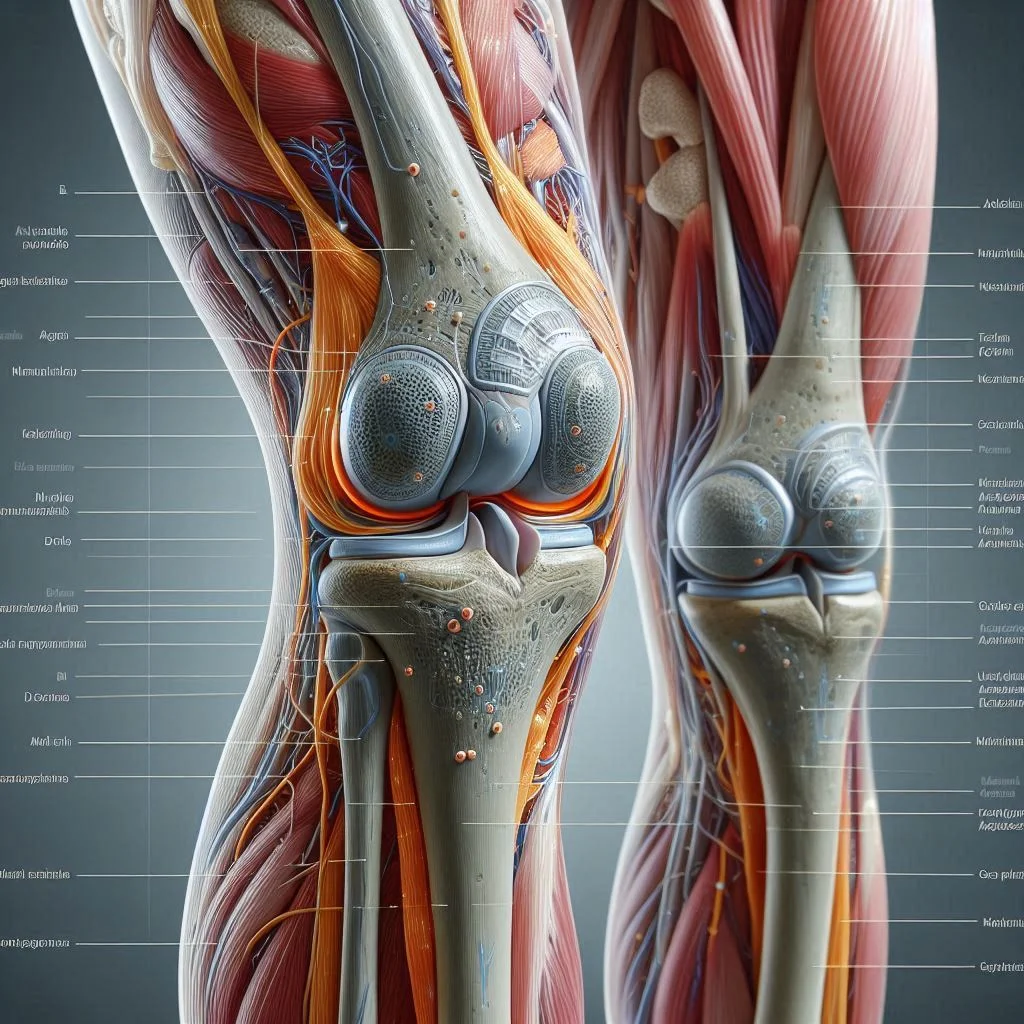
One of the most common reasons for a popping sound in the knee joint centers around harmless gas bubbles forming within the synovial fluid. When you flex or extend your knee, pressure changes inside the joint can cause these gas bubbles to quickly collapse or burst, resulting in an audible pop or cracking sound.
This is very similar to what happens when you intentionally "crack" your knuckles. The popping or cracking sound associated with gas bubbles is normal, not typically accompanied by knee pain, and doesn’t cause damage to cartilage or ligaments.
Biomechanically, tendons or ligaments that cross the knee can occasionally "snap" or shift slightly as you move, especially if you quickly change positions. This may create a popping or clicking sensation at the side of the knee or near the kneecap, again usually without pain or injury. Such noises become more pronounced with age or if there’s a slight imbalance in tracking, but these occurrences are not typically signs of anything problematic on their own.
If you're looking for practical ways to support your knees and reduce discomfort, incorporating targeted chair exercises can be especially beneficial for seniors or anyone seeking gentle mobility improvements. Discover a range of simple routines in this guide to chair exercises for stronger knees that can help you maintain joint health and flexibility at home.
Knee Popping and Knee Pain: When Is It a Sign of Injury?
The combination of knee popping and knee pain deserves closer attention. If you experience popping that is accompanied by pain, swelling, limited movement, or a feeling that your knee won’t "stay put," you might be facing structural injuries inside the knee joint.
For instance, a sudden twist or impact can lead to a meniscus tear, where a piece of cartilage is torn or displaced, causing a painful popping or locking of the knee. Similarly, cartilage damage or cartilage wear from repetitive activities or aging can result in uncomfortable popping sounds as the roughened surfaces rub together.
Prompt evaluation by a knee specialist or orthopedic surgeon is essential when knee popping begins after a clear knee injury or is partnered with persistent knee pain, buckling, giving out, or swelling. Early diagnosis can prevent the problem from worsening, minimize complications, and help you resume your previous level of activity.

Meniscus Tear and Cartilage Damage: Understanding Knee Pop Risks
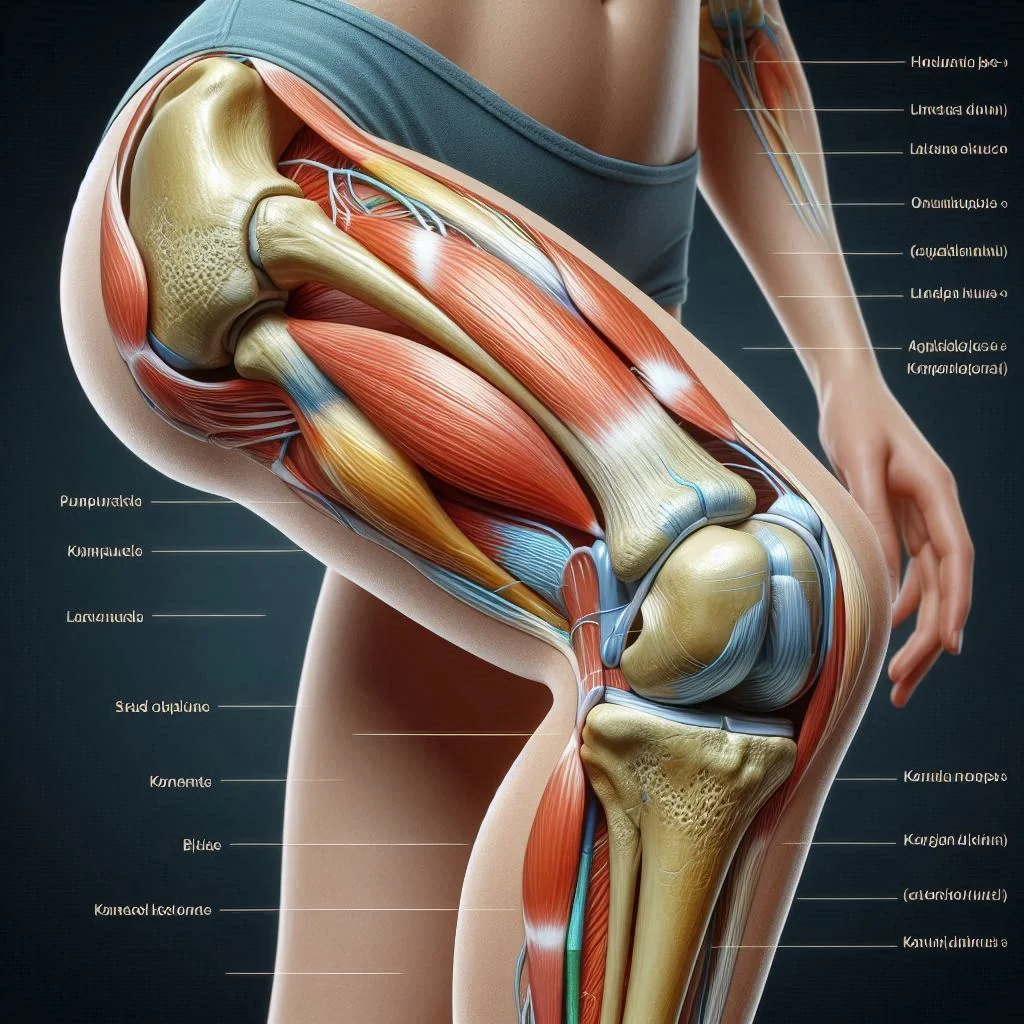
A meniscus tear is a frequent cause of a pronounced popping sound—especially among athletes or those who “twist” their knee during movement. The meniscus is a cushion of cartilage that acts as a shock absorber between your thigh bone and shin bone. When it tears, it can create a popping or clicking noise, often followed by inflammation and knee pain.
On the other hand, chronic cartilage damage or loss (“osteoarthritis”) can cause the joint surfaces to become rough, which similarly results in abnormal sounds, sensations, and possibly a feeling that the knee must "pop back into place" after movement.
Both conditions necessitate evaluation by an orthopedic surgeon or knee specialist and may require advanced imaging such as MRI. Structured physical therapy, anti-inflammatory medications, or even arthroscopic surgery could be recommended depending on the extent of the injury.
Ligament or Tendon Issues: Why Knee Pops with Instability
When a ligament or tendon supporting the knee joint is overstretched or torn—due to sports, a fall, or sudden directional change—the knee can emit a loud pop at the moment of injury. Anterior cruciate ligament (ACL) or medial collateral ligament (MCL) tears often present with an unmistakable "pop," rapid swelling, and immediate loss of function or joint stability. Likewise, snapping tendons, while less common, can produce notable popping sensations if the alignment of bone and connective tissue is disturbed.
These injuries require prompt and expert guidance from a knee specialist or orthopedic surgeon to prevent further joint damage, restore function, and ensure optimal recovery. Rehabilitation may include bracing, targeted physical therapy, or in severe cases, surgical reconstruction.
Referrals to Knee Specialist or Physical Therapist
If you’re concerned about knee popping—especially when it’s accompanied by pain, swelling, or limited mobility—it’s wise to schedule an appointment with a knee specialist or orthopedic surgeon. Early intervention ensures proper diagnosis and tailored treatment, leading to faster, safer healing and prevention of future problems.
Referrals to a licensed physical therapist can provide personalized exercise programs, correct mechanical imbalances, and strengthen muscles supporting your knee—often helping reduce or eliminate bothersome popping sensations.
Remember, even if your symptoms seem minor or come and go, a professional evaluation provides peace of mind and can keep you active and pain-free. Don’t hesitate to seek guidance if something “doesn’t feel right” about your knee pop.
Why Does Knee Pop? Differentiating Normal vs Concerning Knee Popping
Type of Knee Pop |
Common Causes |
When to Seek Help |
|---|---|---|
Occasional painless pop |
Gas bubbles, normal movement |
No medical action needed |
Repeated/with pain |
Cartilage damage, meniscus tear |
See an orthopedic surgeon |
Acute popping after injury |
Ligament or tendon tear |
Urgent medical attention |
Popping Sound Patterns: What to Monitor
Tracking your popping sound patterns can help you determine if your symptoms are normal or in need of attention. Occasional or random pops—especially those unaccompanied by pain—are typically benign and related to gas bubbles or normal movement around a bony prominence.
However, persistent or repetitive pops, especially those associated with locking, catching, or a sensation of the knee shifting, may indicate underlying problems such as cartilage damage or a tear in the meniscus.
If you hear a sudden pop during an injury, especially when you’re unable to bear weight or your knee immediately swells, seek urgent medical help. Orthopedic specialists and sports medicine doctors warn that ignoring persistent popping sounds accompanied by pain can worsen injuries and even lead to chronic instability or arthritis in the joint.
"If knee popping is accompanied by swelling or instability, have it evaluated by a knee specialist right away." – Dr. Michael Patel, Sports Medicine Specialist

Case Studies: Real Patient Stories on Why Does Knee Pop?
Case 1: Young athlete with meniscus tear
A 21-year-old soccer player felt a sharp pop during a game after twisting her knee while pivoting. She developed swelling and couldn’t fully straighten her leg. MRI confirmed a meniscus tear; after arthroscopic surgery and focused physical therapy, her popping subsided, and she returned to sport within a few months.Case 2: Senior experiencing cartilage damage
A 68-year-old retiree described frequent popping with mild knee pain that worsened over a year. X-rays showed cartilage thinning and early arthritis. Her care plan involved low-impact exercise, weight management, and anti-inflammatories. With time, her symptoms improved, and she avoided surgery.Case 3: Desk worker with gas bubbles and no injury
A 35-year-old office worker noticed knee popping every time he stood up but never experienced pain or swelling. Orthopedic evaluation ruled out injury. He was reassured it was harmless—likely related to synovial fluid gas bubbles—not requiring any treatment.

Diagnosing the Cause of Knee Popping: What Orthopedic Surgeons and Knee Specialists Do
Examinations and Imaging for Knee Pop Issues
If you schedule an appointment for knee popping or knee pain, your first visit will usually start with a detailed medical history: when did the pops begin, what triggers them, are they ever accompanied by pain or swelling, and have you had any recent knee injuries? The orthopedic surgeon will then perform a thorough physical exam—checking range of motion, joint stability, ligament integrity, and looking for tenderness or abnormal swelling.
Depending on findings, X-rays may reveal cartilage wear or arthritis, while MRI scans are used to evaluate soft-tissue injuries such as a meniscus tear, cartilage damage, or a torn ligament or tendon. Sometimes, additional tests such as ultrasound or CT are used if structural abnormalities are suspected but not visualized by standard imaging. The goal is a precise diagnosis so treatment is timely and effective, preventing further knee joint issues or chronic knee pain.
Role of the Physical Therapist in Knee Popping and Knee Pain
Physical therapists are key allies when knee popping does not involve major injuries requiring surgery. After assessment, they may recommend strengthening exercises for the quadriceps, hamstrings, and hip muscles to support optimal knee mechanics and reduce abnormal movement patterns causing a popping sensation. They also teach flexibility and balance routines, address gait or alignment problems, and help patients regain full range-of-motion after injury or surgery.
With dedicated physical therapy, many people can achieve noticeable improvement in knee popping, eliminate joint pain, and decrease the risk of future injuries. If the physical therapist observes concerning findings—such as ongoing instability or worsening symptoms—they will refer you back to your knee specialist or orthopedic surgeon for re-evaluation.

Watch this medical animation to see how gas bubbles, cartilage, and ligaments can contribute to knee popping, and learn more about when you should seek expert advice.
Treatment Options: What to Do About Knee Popping
Home Remedies and Self-Care for Minor Knee Pop
For mild or occasional knee popping not associated with pain or injury, self-care can be effective. Gentle stretching, maintaining flexibility, and strengthening muscles around the knee joint can reduce abnormal popping. Simple actions like warming up before activities, ensuring proper walking and squat technique, wearing supportive shoes, and avoiding repetitive high-impact movements can help. Staying active and maintaining a healthy weight reduce stress on the joints, decreasing underlying causes of popping.
If your popping gets worse, becomes frequent, or starts being accompanied by pain or swelling, stop any aggravating activities and consult a knee specialist for guidance. Over-the-counter anti-inflammatories may temporarily relieve discomfort, but it’s always best to identify the true cause before proceeding with any treatment plan.
Medical Treatments for Cartilage Damage, Meniscus Tear, and Ligament Issues
Injuries like cartilage damage, meniscus tear, or ligament or tendon strain typically require more structured care. Depending on the diagnosis, treatment options may include:
Prescription anti-inflammatories to reduce swelling and pain
Physical therapy to restore strength and function
Bracing or taping for extra joint support
Minimally invasive arthroscopic surgery to repair or remove torn tissue
Platelet-rich plasma (PRP) or other regenerative procedures for select cartilage or tendon injuries
Your orthopedic surgeon will personalize your treatment plan to help you recover safely and quickly. In most cases, non-surgical options are effective, especially when combined with expert advice and a tailored rehabilitation program.
"Physical therapy and targeted exercises can alleviate pain and prevent further popping in most cases." – Dr. Heather Simons, Licensed Physical Therapist
Preventing Knee Pop: Expert-Recommended Tips and Strategies
Warm up and stretch before activity
Strengthen supporting muscles
Maintain healthy weight
Avoid high-risk movements for your joint health
People Also Ask: Why Does Knee Pop?
How do you fix knee popping?
Answer: Treatment for knee popping depends on the underlying cause. Minor popping with no pain may require strengthening exercises, stretching, and ensuring proper movement patterns. If pain or swelling is involved, consult an orthopedic surgeon or knee specialist for a personalized assessment. Persistent knee popping related to an injury (like a meniscus tear or cartilage damage) may require medical intervention, ranging from physical therapy to surgery.
Should I be worried if my knee pops?
Answer: Most knee popping is harmless—especially if it's painless and not associated with injury or swelling. However, if your knee pops frequently and is accompanied by pain, locking, or instability, see a knee specialist or an orthopedic surgeon to rule out conditions like meniscus tears or ligament/tendon injuries.
Frequently Asked Questions: Why Does Knee Pop?
Is knee popping always a sign of damage? Not necessarily. Most knee popping is harmless and due to gas bubbles or normal tissue movement. Persistent or painful popping could signal injury—see a medical professional for guidance.
Can I prevent my knee from popping? Regular exercise, stretching, strengthening supporting muscles, and avoiding aggravating activities can help reduce abnormal knee popping. Optimizing your joint health reduces risk.
Are there long-term risks to ignoring knee popping? Ignoring popping that is accompanied by pain or follows an injury can increase your risk for worsening joint damage or chronic instability. Always get persistent symptoms checked.
Key Takeaways: Why Does Knee Pop? What You Need to Remember
Knee popping is common and usually benign, but persistent or painful popping might indicate an injury.
Gas bubbles, cartilage wear, ligament injuries, and meniscus tears are the major causes of knee popping.
A qualified orthopedic surgeon or knee specialist can provide an accurate diagnosis and treatment plan.
Ready to Take Control of Your Joint Health? Schedule a Consultation with a Knee Specialist Today!
Don't let knee popping or knee pain keep you from your favorite activities or future mobility. If you have questions or concerns, a personalized evaluation from a board-certified orthopedic surgeon or knee specialist is your best next step.
Your joint health matters—take action today!
If you’re committed to improving your overall mobility and managing joint discomfort, it’s important to look beyond just the knees. Many people find that strengthening the glutes can play a pivotal role in supporting healthy movement and reducing arthritis-related pain throughout the lower body.
For a deeper dive into how targeted glute exercises can enhance your mobility and complement your knee care routine, explore these top glute exercises for arthritis and unlock new strategies for lasting joint health.
Sources
OrthoInfo – https://orthoinfo.aaos.org/en/diseases--conditions/knee-pain/
Mayo Clinic – https://www.mayoclinic.org/diseases-conditions/knee-pain/
Harvard Health – https://www.health.harvard.edu/pain/knee-pain
Understanding the causes of knee popping is essential for maintaining joint health and knowing when to seek medical attention. For a comprehensive overview, consider reading “What Does a Pop in Your Knee Mean?” by the Hospital for Special Surgery, which explains various reasons behind knee popping and when it might indicate a problem.
In addition, “Knee Popping and Pain: Causes and When to Consult a Doctor” from Medical News Today offers insights into common causes and advises on when to seek medical advice. If you’re serious about understanding and addressing knee popping, these resources will provide valuable information and guidance. NCWellnessHub.com
 Add Row
Add Row  Add
Add 




Write A Comment