Do studies show most chronic lower back pain patients can get relief without going under the knife? If you’re facing the possibility of lumbar fusion, you’re not alone
A Breakdown of Non-Surgical and Minimally Invasive Options for Chronic Lower Back Pain
Anyone suffering from chronic back pain knows just how much it can limit your quality of life, affecting everything from work to family activities. Despite the prevalence of spine surgery for lower back issues, more and more specialists—from orthopedic surgeons to neurosurgeons and physical medicine doctors—urge patients to try multiple alternatives to lumbar fusion first.

The clinical pathway recommended by most expert guidelines involves starting with physical therapy, continuing through pain-relieving injections, and only considering spinal fusion surgery if these less invasive interventions fail to provide lasting relief or if there is significant spinal instability.
In this article, we’ll explore those alternatives in detail, examine scientific evidence behind each option, and provide clear, practical advice on building a personalized treatment plan in partnership with your healthcare team.
Our guide includes the latest peer-reviewed research and clinical insights from authoritative sources including the PubMed, Cleveland Clinic, the Mayo Clinic, and the Spine Journal.
You’ll also find expert commentary and real-world advice for people navigating conditions like degenerative disc disease, spinal stenosis, and spondylolisthesis. If you’re seeking reliable, unbiased information on fusion alternatives, you’re in the right place.

The State of Spinal Health: Why Explore Alternatives to Lumbar Fusion?
Americans face an epidemic of lower back pain—a leading cause of disability and missed work days. According to the Spine Journal (2023):
“According to spine specialists, over 400,000 spinal fusion surgeries are performed annually in the US, yet most patients are recommended to exhaust alternatives to lumbar fusion first.”
Despite the high prevalence of fusion surgery, multiple studies indicate that a significant percentage of patients experience ongoing pain or dissatisfaction after spinal fusion. With advances in non-surgical and minimally invasive spine surgery, there are now more surgical alternatives to lumbar fusion than ever.
Common conditions like spinal stenosis, herniated disc, or degenerative disc disease may improve with conservative management or targeted minimally invasive options. By seeking out these alternatives first, patients can often maintain better range of motion and speed up their recovery time, delaying or avoiding surgery altogether.
What You'll Learn About Alternatives to Lumbar Fusion
Clinical evidence for avoiding spinal fusion surgery
Non-surgical and minimally invasive alternatives to lumbar fusion
Specific alternatives for conditions like spinal stenosis, disc disease, and degenerative disc disease
Guidelines on when lumbar fusion is warranted
Risks, limitations, and expert tips for a personalized treatment plan
Understanding Lumbar Fusion and Its Limits
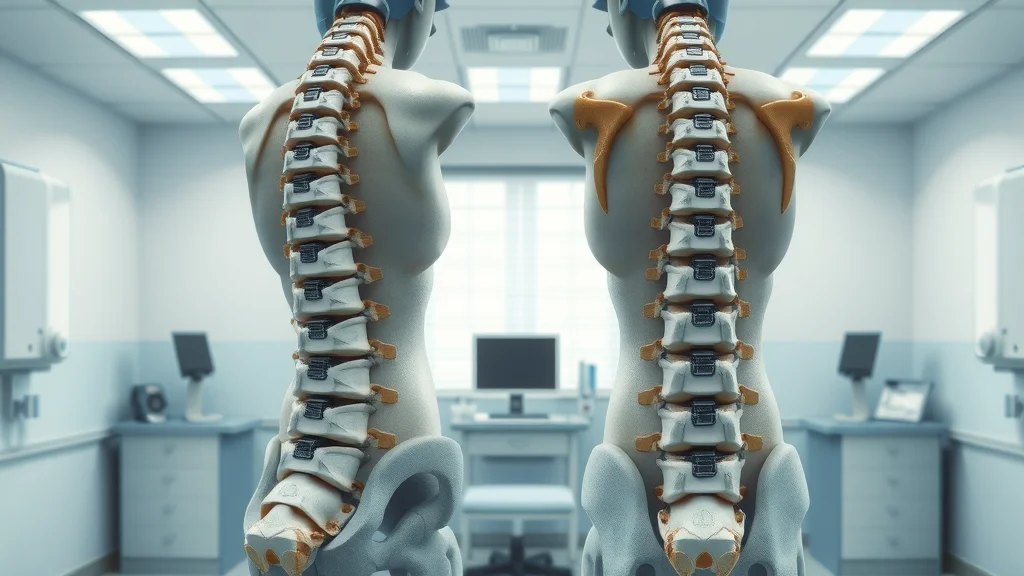
Before diving into alternatives to lumbar fusion, it’s important to understand what lumbar fusion is, why it’s performed, and its limitations. Lumbar fusion is a procedure in which two (or more) vertebrae in the lower spine are permanently joined together, often with surgical hardware, to stabilize the spine and reduce pain.
While it can be effective for specific problems—such as severe instability, major spinal deformities, or unmanageable pain—the risks and long recovery associated with fusion mean it’s not the best option for everyone.
Recent research highlights drawbacks including limited range of motion, potential for adjacent segment disease (where nearby discs degenerate faster), and a notable “regret rate” where up to 40% of fusion patients report ongoing pain or dissatisfaction. That’s why top spine surgeons and clinical guidelines increasingly treat fusion as a last resort.
When is Lumbar Fusion Surgery Recommended?
Spinal fusion surgery is typically reserved for patients who present with severe spine instability, progressive neurologic deficits, or those who have not responded to comprehensive non-surgical care. According to experts at the Cleveland Clinic, indications can include:
Spinal fractures with instability
High-grade spondylolisthesis (vertebrae slipping out of place)
Significant spinal deformity (such as scoliosis)
Failed back surgery syndrome with severe, unremitting pain
Tumor or infection requiring stabilization
Risks, Recovery Time, and Why Patients Seek Alternatives to Lumbar Fusion
While fusion surgery can offer life-changing relief in select cases, it comes with notable risks: infection, blood clots, nerve damage, persistent pain, and the possibility of hardware failure. The recovery time is significant—often ranging from 6 months to a year for full function, and many patients experience loss of flexibility and ongoing discomfort. Concerns about quality of life post-fusion along with the risk of “adjacent segment disease” (where other levels of the spine wear out faster) motivate many patients to seek fusion alternatives before surgery become necessary.
According to clinical guidelines and the Mayo Clinic, “Most cases of chronic back pain improve with conservative treatment”—and surgery is considered only when those options fail. That’s why leading specialists recommend a stepwise approach, reserving fusion for the rare cases where it’s clearly the only way to address the underlying spine stability or severe neurologic deficits.
Who Is (and Isn’t) a Candidate for Alternatives to Lumbar Fusion?
Ideal candidates for alternatives to lumbar fusion are those with chronic back pain without major instability, fractures, rapidly worsening nerve damage, or structural conditions threatening spinal stability. This includes many patients with degenerative disc disease, mild spondylolisthesis, herniated discs, or spinal stenosis—conditions that frequently improve with non-surgical interventions or minimally invasive procedures. However, people with severe deformity, bone tumors, infection, or progressive neurological loss may not benefit from alternatives and are often surgical candidates.
If you’ve exhausted conservative treatments like physical therapy and injections without improvement and have imaging showing progressive instability or significant nerve compromise, a surgical option may be warranted. Your spine specialist will use imaging, neurological exams, and a detailed review of your case to guide you toward the most appropriate, individualized treatment plan.

Conservative Care First: Clinical Guidelines for Back Pain and Lower Back Conditions
According to modern clinical guidelines, all patients should exhaust conservative care approaches before considering lumbar fusion or other invasive spine surgery. Multiple well-controlled studies published in Spine Journal and JAMA demonstrate that non-surgical care—including physical therapy, exercise, activity modification, medications, or pain-relieving injections—leads to significant improvement for most with chronic lower back pain. Only if conservative management fails to provide adequate pain relief and function, and if there is confirmed underlying pathology, is surgery considered.
This essential “stepwise approach” dramatically reduces unnecessary surgery and prioritizes patient safety and function. It’s also why insurance companies and expert medical panels now require documentation of failed conservative care before authorizing elective lumbar fusion.
For those interested in a holistic approach to pain management, exploring complementary therapies can be a valuable addition to your treatment plan. Techniques such as mindfulness, acupuncture, and other integrative methods have shown promise in reducing pain and improving quality of life—discover more about these options in our guide to complementary therapies for reducing pain.
Physical Therapy and Rehabilitation: Foundation of Alternatives to Lumbar Fusion
Physical therapy is the cornerstone of any conservative back pain management plan. Professionally supervised physical therapy builds core strength, improves flexibility, and teaches safe body mechanics, resulting in pain reduction and functional improvement. The American Academy of Orthopaedic Surgeons reports that 80–90% of patients with chronic lower back pain see substantial improvement with regular, targeted rehabilitation.
A spine-specific physical therapy program may include:
Core stabilization and muscle strengthening
Stretching for the lumbar spine, hips, and legs
Manual therapy (e.g., massage, mobilizations)
Education about posture, ergonomics, and movement habits
Modalities such as heat, ice, or electrical stimulation for pain

Medications and Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
Medications play a key short-term role in managing symptoms during flare-ups of chronic back pain or acute injuries. Over-the-counter NSAIDs (like ibuprofen or naproxen) work by reducing inflammation and providing pain relief, while prescription medicines—such as muscle relaxants, topical analgesics, or certain antidepressants—may help with chronic nerve pain or muscle spasms.
Spine specialists caution that medications should rarely be the only mode of treatment. They are best used alongside physical therapy or activity changes as part of a larger recovery plan. Opioids and strong prescription painkillers are reserved for short periods only, due to risks of dependence and adverse side effects. Always consult your healthcare provider before starting, changing, or stopping any medication for lower back issues.
Injections for Lower Back Pain: Epidural Steroids, Nerve Blocks, and More
For those whose back pain persists after physical therapy and medications, image-guided spinal injections may offer relief. Popular injection therapies include:
Epidural steroid injections: Reduce inflammation and swelling around spinal nerves, helpful for disc herniations or sciatica
Nerve blocks: Numb pain pathways at specific joints or nerves involved in chronic pain
Facet joint injections: Target inflammation in the small joints along the back of the spine
Radiofrequency ablation: Temporarily disables pain-carrying nerves for months at a time
Comparison of Conservative Alternatives to Lumbar Fusion: Effectiveness, Duration, and Common Indications
Treatment Option |
Effectiveness |
Duration of Relief |
Typical Indications |
|---|---|---|---|
Physical Therapy |
70-90% benefit |
Months to years (with ongoing exercise) |
Back pain, degenerative disc, mild spondylolisthesis |
NSAIDs & Medications |
60-70% benefit (short-term) |
Days to weeks |
Acute flare-ups, chronic pain |
Injections (Epidural, Facet, Nerve Block) |
50-80% temporary relief |
Weeks to months |
Herniated disc, radiculopathy, spinal stenosis |
Minimally Invasive Spine Surgery: Modern Fusion Alternatives for Chronic Back Pain
If conservative care does not achieve adequate pain control or restore function, minimally invasive spine procedures can offer fusion alternatives for certain conditions. Unlike traditional open surgery, these techniques use small incisions, specialized instruments, and real-time imaging to repair damaged tissues or decompress nerves while preserving most of the spine’s structural integrity.
Benefits include less postoperative pain, shorter recovery, and better preservation of range of motion. According to the Mayo Clinic, the majority of patients return to daily activities sooner compared to those undergoing fusion.
Not every patient with chronic lower back pain is eligible for minimally invasive procedures, but for many with herniated disc, mild spinal stenosis, or limited degenerative changes, these options provide relief while allowing patients to delay or avoid fusion.

Microdiscectomy, Laminectomy, and Decompression Surgery as Alternatives to Lumbar Fusion
Common minimally invasive surgeries include:
Microdiscectomy: Removal of part of a herniated disc pressing on spinal nerves, performed through a small incision with a microscope
Laminectomy: Removal of a small section of bone (lamina) to relieve pressure in spinal stenosis
Minimally invasive decompression: Extraction or shaving of tissue compressing nerves or the spinal cord without destabilizing the spine
Importantly, these procedures are only recommended when non-surgical methods haven’t worked and when imaging confirms the need for intervention. They do not provide stability in cases of major deformity, instability, or severe spondylolisthesis—scenarios where fusion surgery might still be required.
Endoscopic Spine Surgery: A New Minimally Invasive Option
Advances in technology have introduced endoscopic spine surgery, where a miniature camera and fine instruments are inserted through tiny incisions. This option allows surgeons to address disc herniations or localized stenosis with minimal disruption to muscles and ligaments.
Patients choosing endoscopic options report less postoperative pain, a shorter hospital stay, and a much quicker return to activity than traditional fusion. While not suitable for those with severe instability or multi-level disease, endoscopic techniques are expanding treatment options for those seeking an effective fusion alternative for chronic back issues. Discuss with your specialist whether this newer minimally invasive option fits your diagnosis and goals.
Artificial Disc Replacement: A Leading Alternative to Lumbar Fusion
For many patients, the most advanced alternative to spinal fusion is artificial disc replacement. This modern surgical option involves removing a worn or damaged disc in the lower spine and replacing it with an artificial, motion-preserving implant. Unlike fusion—where motion at the affected level is lost—disc replacement allows continued flexion, bending, and rotation, which can help maintain quality of life and reduce adjacent segment disease.
Disc replacement is especially beneficial for selected younger, active adults with isolated degenerative disc disease or certain types of herniated discs. According to multiple peer-reviewed studies, disc replacement has similar or better pain outcomes and lower rates of adjacent segment problems compared to fusion for properly selected patients.

What Is Artificial Disc Replacement and How Does It Preserve Range of Motion?
Artificial disc replacement is a specialized surgery where the damaged lumbar disc causing chronic pain is removed and replaced with a carefully engineered prosthetic. Unlike fusion surgery, which joins vertebrae together and eliminates movement at that level, disc replacement devices are built to mimic the natural movement (“range of motion”) of a healthy spinal disc.
By preserving mobility of the lumbar spine, artificial disc replacement reduces the risk that other spinal segments will “wear out” prematurely. Clinical trials demonstrate that patients retain better forward bending, extension, and rotation than those who undergo fusion—making disc replacement a top fusion alternative for those who qualify. Your surgeon will weigh factors like age, spine health, and the underlying diagnosis before recommending this advanced treatment option.
Disc Replacement Outcomes for Degenerative Disc Disease and Herniated Disc
Multiple studies, including those published by the Mayo Clinic and New England Journal of Medicine, have found that artificial disc replacement leads to pain reduction and improvement in function equal to or greater than fusion surgery—with the added benefit of preserved mobility. Common conditions treated include isolated degenerative disc disease without significant facet joint arthritis or spinal instability and certain one-level herniated discs.
Long-term results show lower rates of adjacent segment degeneration, less need for secondary surgeries, and faster recovery in the majority of patients. However, not every patient is a good candidate: advanced arthritis, osteoporosis, or multi-level disease may preclude disc replacement, and insurance coverage can vary. Always consult a spine specialist trained in both fusion and artificial disc options to plan your treatment.
Fusion Surgery vs. Artificial Disc Replacement: Mobility, Recovery Time, and Long-term Results
Feature |
Fusion Surgery |
Artificial Disc Replacement |
|---|---|---|
Mobility at Treated Level |
Lost (fused) |
Preserved |
Recovery Time |
6–12 months |
2–6 weeks |
Risk of Adjacent Segment Disease |
Increased |
Lowered |
Long-term Pain Relief |
60–80% (may vary) |
70–90% (in selected patients) |
Condition-Specific Alternatives: Options for Spinal Stenosis, Spondylolisthesis, and Disc Disease
Not all spine conditions require the same treatment plan. Here are key alternatives for common diagnoses:
Spinal Stenosis: When Decompression and Non-Fusion Treatments Are Preferred
Spinal stenosis (narrowing of the spinal canal) often causes sciatica, leg cramps, or walking difficulty. Current guidelines recommend starting with physical therapy and anti-inflammatory medications. If these fail, decompression surgery (removing bone or tissue pinching the nerves) without fusion can relieve symptoms in many. The majority of older adults with mild to moderate lumbar stenosis get effective, long-lasting pain relief from decompression, with far fewer risks and faster recovery than with instrumentation and fusion.
Fusion is only considered for severe, unstable, or fixed deformities—the minority of cases. Seek a specialist well versed in both surgical and nonsurgical treatment options for the best outcomes and to minimize unnecessary procedures.
Spondylolisthesis and Degenerative Disc Disease: Personalized Treatment Plans
Mild to moderate spondylolisthesis (vertebra slipping forward) and most cases of degenerative disc disease are best managed first with conservative therapies: physical therapy, weight management, activity modification, and sometimes targeted injections.
Only high-grade spondylolisthesis, severe instability, or progression of neurologic symptoms despite non-surgical intervention would warrant fusion or a motion-preserving procedure like disc replacement.
Personalized plans based on imaging, symptoms, and your goals prioritize function, mobility, and safety. Collaboration between you and your spine team is key—a “one size fits all” approach is rarely effective.

Selecting the Right Treatment Option Based on Your Back Pain Diagnosis
There is no single “best” alternative to lumbar fusion for every patient. The right treatment plan depends on:
Underlying diagnosis (disc disease, spinal stenosis, spondylolisthesis, etc.)
Imaging findings and stability of the lumbar spine
Your age, activity level, goals, and other health conditions
Previous treatments attempted and their outcomes
pain reliefquality of life
Risks, Limitations, and When Lumbar Fusion Remains Necessary
Although alternatives to lumbar fusion are highly effective for many, some cases require traditional fusion surgery as the only viable solution. Major red flags that may force surgery include rapidly progressing neurologic loss (like drop foot), major structural instability, vertebral collapse, infection, aggressive tumors, or traumatic injuries. Ensuring a thorough, individualized evaluation by a spine specialist is crucial.
“Clinical guidelines suggest lumbar fusion should be reserved as a last resort—after all other alternatives have been exhausted and when structural spinal stability is threatened.” — Dr. Amy Park, Neurosurgeon
fusion surgery
Recognizing Non-Candidates for Alternatives to Lumbar Fusion
Some patients—such as those with significant spine deformity, advanced osteoporosis, severe spondylolisthesis, vertebral fractures, cancer, or infection—are unlikely to benefit from fusion alternatives. In these scenarios, prompt traditional surgery is often necessary to preserve neurologic function and prevent worsening disability. Patients with rapid neurologic deterioration—numbness, progressive weakness, loss of bladder/bowel control—require immediate evaluation and urgent surgical intervention.
If your symptoms don’t improve after several months of best-practice conservative care or they worsen, advanced imaging and a surgical consult are warranted. The key is ongoing communication with a multidisciplinary team.

Clinical Red Flags: Progressive Neurologic Deficit, Instability, and Severe Cases
Always seek medical attention if you experience:
Sudden, severe or rapidly worsening back/leg pain
Loss of muscle strength, foot drop, or balance issues
Loss of sensation around the groin or legs (“saddle anesthesia”)
Changes in bladder/bowel control
Persistent pain after trauma
People Also Ask About Alternatives to Lumbar Fusion
Can you avoid spinal fusion surgery?
Most cases of chronic lower back pain improve with alternative treatments to lumbar fusion such as physical therapy, injections, medications, or minimally invasive procedures. However, surgery is advised only when these options fail and/or there are severe structural issues.
What is the new spinal fusion technique?
Newer spinal fusion techniques include minimally invasive fusion surgery and novel hardware approaches, but these are typically reserved for patients not responding to less invasive alternatives to lumbar fusion.
What is the hardest joint replacement surgery to recover from?
Recovery from spine surgery—particularly fusion or disc replacement—can be longer than recovery from joint replacement of the hip or knee, and is highly patient-specific depending on the extent of surgery and preexisting spine health.
What percentage of people regret spinal fusion?
Estimates vary, but studies cited by Mayo Clinic and Cleveland Clinic find 20-40% of patients report ongoing pain or dissatisfaction after lumbar fusion, underscoring the importance of considering all alternatives first.

Frequently Asked Questions: Alternatives to Lumbar Fusion
Is artificial disc replacement safer than fusion?
How do you know if you qualify for a minimally invasive alternative?
What are the long-term outcomes of avoiding lumbar fusion?
What costs are involved with alternatives to lumbar fusion?
Key Takeaways: Alternatives to Lumbar Fusion
Most patients benefit from trying conservative treatments and minimally invasive options before considering lumbar fusion.
Discuss all alternatives to lumbar fusion with your spine specialist for a personalized, condition-specific plan.
Clinical guidelines reserve spinal fusion for severe, structurally unstable or unresponsive cases.

Conclusion: Making Informed Decisions About Alternatives to Lumbar Fusion
Making an informed decision about alternatives to lumbar fusion means understanding your condition, considering conservative and minimally invasive treatments, and working closely with a specialist to develop the best individualized plan for you.
How to Consult with a Spine Specialist and Develop Your Individualized Treatment Plan
Start with a comprehensive evaluation by an orthopedic spine surgeon, neurosurgeon, or physical medicine doctor experienced in fusion alternatives. Request a multidisciplinary review of your imaging and symptoms. Ask about the risks, benefits, and expected outcomes of each treatment option.
Only move to fusion surgery after all conservative and less invasive options have been explored or if your specialist determines it’s essential for your spinal stability or neurological function.
Explore more unbiased, expert-reviewed health guides at NCWellnessHub.com.
If you’re interested in how innovative care models are transforming patient outcomes beyond the operating room, you might find it valuable to explore the evolving landscape of hospital-level care delivered at home.
This new paradigm is reshaping recovery, comfort, and family involvement for patients of all ages. For a deeper look at how healthcare is adapting to meet modern needs—especially for children and families—read our feature on hospital care at home for kids.
Discover how these advancements could influence your own approach to healing and wellness, and gain insight into the future of patient-centered care.
 Add Row
Add Row  Add
Add 




Write A Comment