"Fatigue is not just tiredness—it's an all-consuming drain." Understanding how osteoarthritis contributes to relentless exhaustion is the first step toward regaining control over your daily life and wellbeing. In this comprehensive guide, we’ll explore exactly why living with osteoarthritis (OA) can leave you feeling utterly wiped out—and more importantly, what you can do about it to boost your energy, sleep better, and feel like yourself again.

What You'll Learn from This Guide on Does Osteoarthritis Cause Fatigue
The connection between osteoarthritis and fatigue
Sleep quality concerns in osteoarthritis
How pain and depression can contribute to fatigue
Tips to manage fatigue and improve physical function
The impact of knee osteoarthritis on daily life
Dietary considerations and lifestyle changes
"Fatigue is not just tiredness—it's an all-consuming drain." Understanding Fatigue and Osteoarthritis
Fatigue in osteoarthritis (OA) is fundamentally different from common tiredness, often linked to chronic pain, impaired physical function, and other side effects. Many patients with osteoarthritis notice that fatigue can feel like a deep energy deficit—one that doesn’t improve with a simple nap or a good night’s rest. This persistent lack of energy significantly affects the quality of life for people dealing with OA.
Research shows a strong relationship between fatigue and other common osteoarthritis symptoms such as chronic pain, joint stiffness, and impaired physical function. In fact, the physical function challenges that come with OA can contribute to a cycle of pain, poor sleep, and chronic exhaustion, which often overlap and exacerbate each other. Recognizing this connection is vital for both patients with OA and their caregivers, as fatigue is a significant side effect that impacts daily life and overall quality of life.
For those living with knee osteoarthritis or other joint involvement, these fatigue levels can spike during flare-ups or periods of increased disease activity. Additional factors—like sleep disorders, inflammation, pain and depression, and the ongoing stress of managing a chronic health condition—act as side effects that worsen overall functioning. By acknowledging that fatigue is more than just tiredness, individuals with knee osteoarthritis and other health conditions can better advocate for comprehensive care that addresses sleep problems and improves quality of life.

Exploring the Link: Does Osteoarthritis Cause Fatigue?
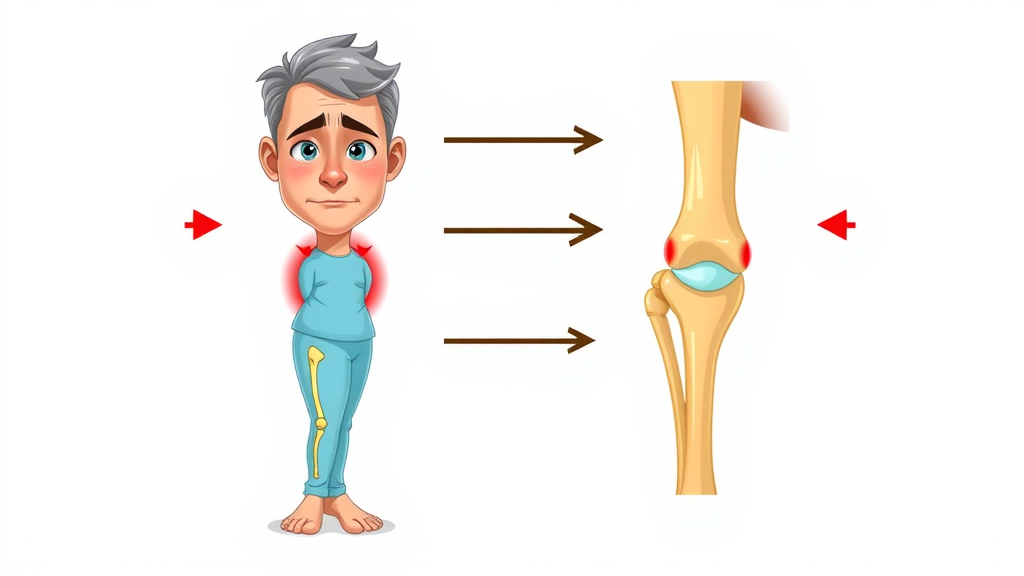
So, does osteoarthritis cause fatigue? Current medical understanding confirms that osteoarthritis often causes pronounced fatigue, a side effect that extends beyond normal tiredness and significantly affects sleep quality and physical function. Several mechanisms underlie this link, including chronic pain, inflammation, disease activity, and sleep problems that collectively impact sleep quality and physical function. OA is a chronic disease that involves not only degeneration of joint cartilage but also systemic changes, like ongoing inflammation, immune system activation, and sleep disruption. These biological processes physically and mentally drain individuals, making even routine daily activities unusually challenging.
Further, research shows that the relationship between fatigue and osteoarthritis is multidimensional. Studies highlight the impact of chronic pain, reduced physical function, and poor sleep quality as central contributors to increasing fatigue levels in people with osteoarthritis and rheumatoid arthritis, emphasizing the complex disease activity involved. For many, this combination leads to a vicious cycle: pain reduces sleep quality, which limits recovery and compounds daytime fatigue, which then further dampens mood and mobility. Whether you have knee osteoarthritis or OA in other joints, understanding these roots of fatigue is essential to managing your health condition holistically.
It's also worth noting that lifestyle factors, including dietary choices, can play a significant role in managing both osteoarthritis symptoms and fatigue. For those interested in how nutrition can influence chronic conditions, exploring how your diet can help manage inflammation and support overall health may offer additional strategies to complement your osteoarthritis care plan.

Osteoarthritis as a Health Condition and Its Symptoms
Osteoarthritis is more than just a joint problem; it is a chronic health condition with multiple side effects including fatigue, chronic pain, and sleep problems that profoundly affect daily life. As a progressive health condition, it causes cartilage breakdown, inflammation, and pain—often in the knees, hips, hands, and spine. Core symptoms include joint pain, tenderness, stiffness (especially after inactivity), and limited movement. Over time, these physical symptoms result in significant side effects, such as fatigue in OA.
Pain often leads to changes in activity levels, reduced muscle strength, and, ultimately, a substantial decline in overall physical function. These functional limitations not only hinder daily life but also increase fatigue levels, making management of physical function and sleep quality essential. Moreover, OA is a chronic disease, meaning symptoms are long-lasting and frequently worsening due to active disease activity, which places ongoing demands on the body’s resources and immune system.
The broad array of symptoms experienced by patients with OA highlights why fatigue is a common side effect. Persistent pain and discomfort make it difficult to stay active, while efforts to compensate for limited mobility often result in expending extra energy for everyday tasks. Psychological side effects—like anxiety or depression—also commonly develop and add another layer to the overall energy drain experienced during life with osteoarthritis.

How Fatigue Differs from Normal Tiredness
One of the most important points for anyone seeking answers to “does osteoarthritis cause fatigue?” is understanding how osteoarthritis-related fatigue differs from normal tiredness, as it is persistent and linked to chronic pain, sleep problems, and disease activity. Whereas regular tiredness is typically temporary and relieved by rest, OA-related fatigue is persistent, affecting both body and mind regardless of the amount of sleep you get.
This type of exhaustion can compromise concentration, motivation, and even mental clarity—making simple decisions or conversations difficult. Importantly, this fatigue in OA is influenced by physiological processes including chronic pain, inflammation, immune system activation, and sleep disturbance—all of which are side effects intimately tied to the disease process itself.
Compounding matters further is the reality that fatigue often overlaps with depression and feelings of hopelessness in OA patients. The result is a feedback loop: feeling persistently drained lowers the desire and ability to engage in physical activity or social events, which in turn reinforces the cycle of fatigue, poor sleep, and functional limitation. Recognizing that this fatigue is a medical symptom—and not a sign of personal failure—can lead to more targeted and supportive healthcare interventions.
"Fatigue affects more than just energy levels—it impacts daily life and quality of life for those managing osteoarthritis."
How Does Osteoarthritis Cause Fatigue? Mechanisms and Contributing Factors
Fatigue in osteoarthritis is driven by several interacting biological, psychological, and lifestyle factors, including chronic pain, sleep problems, and inflammation associated with disease activity. Understanding these mechanisms can empower patients to manage fatigue proactively and have more meaningful conversations with healthcare providers. The complexity of these causes explains why OA fatigue is often severe, persistent, and resistant to simple solutions.
Primary contributors—and the resulting side effects—include chronic pain, ongoing inflammation (a contributing factor to immune system changes and disease activity), and sleep problems. When physical function suffers, so too does the ability to recover and recharge. Furthermore, psychological factors such as depression and anxiety can worsen fatigue, setting off a chain reaction that spills into daylight hours and impacts all aspects of daily life.
Chronic Pain, Inflammation, and Their Role in Fatigue
Chronic pain is a hallmark of OA, and it’s also a primary cause of fatigue in OA patients. The relentless pain signals sent to the brain tax both mental and physical reserves, leading to lower energy output—and this drain persists even when at rest. Beyond pain, chronic, low-grade inflammation plays a major contributing role. Inflammation is the body's response to tissue damage in OA, which leads to the release of inflammatory chemicals called cytokines. These not only drive local pain and swelling but can also affect brain function, disrupting normal sleep habits and sapping overall vitality.
Significantly, the immune system in people with arthritis remains activated, trying to respond to perceived joint threats. This continuous state of alertness leaves the body in a state of "low power," impeding tissue repair and causing elevated fatigue levels. Inflammation and pain can even escalate further during disease flare-ups, explaining why many patients report feeling “completely wiped out” during periods of high disease activity. By viewing fatigue as a side effect of chronic pain and inflammation, healthcare teams are better positioned to offer integrative treatments.

Disease Activity, Sleep Problems, and Sleep Quality
Another key link between osteoarthritis and fatigue is the connection to disease activity, sleep problems, and their combined impact on sleep quality and physical function. Flares or increases in OA-related pain and stiffness typically correspond with an uptick in sleep disturbance—such as staying awake from midnight pain, tossing and turning, or being unable to find a comfortable sleep position. These sleep disruptions reduce quality sleep and prevent the restorative rest needed to repair tissues and restore energy.
Studies have repeatedly shown that poor sleep quality is not only a side effect of OA but also a direct cause of arthritis fatigue. The relationship between fatigue and sleep is bidirectional: pain makes it harder to sleep, but lack of sleep increases pain sensitivity and lower physical function. Over time, this pattern creates a vicious cycle affecting the body’s ability to heal and cope with stress, making good sleep habits a central target for anyone trying to manage fatigue and get back to enjoying daily life.
Physical Function, Pain and Depression, and Energy Drain
Diminished physical function is a common complaint among OA sufferers and is closely tied to higher fatigue levels, which significantly reduce quality of life. When joints are stiff, swollen, or painful, even small physical tasks take more effort. This extra energy expenditure compounds fatigue in OA, reducing the body’s ability to recover and increasing frustration. Studies confirm that people with OA who have greater physical limitations generally report higher levels of fatigue and lower quality of life.
Moreover, pain and depression frequently co-exist with OA. Persistent pain is mentally exhausting; it occupies your thoughts and disturbs your sleep, while depression adds an emotional weight that makes it hard to find motivation. Together, these twin drivers of fatigue reinforce each other, creating ongoing energy deficits and amplifying the impact of other side effects, such as sleep disturbance and immune system changes. Recognizing this interplay is crucial for comprehensive OA management.

Daily Life Disruptions: The Hidden Side Effects
The side effects of OA, especially fatigue, ripple through every aspect of daily life. Fatigue isn’t just an inconvenience—it is a significant side effect that limits mobility, reduces social engagement, and makes routine household tasks feel insurmountable, severely impacting quality of life.
For many, OA-related fatigue also means missing out on favorite activities, decreased participation at work or with family, and a reduced sense of self-worth. This “hidden” side effect is often overlooked compared to joint pain and stiffness, but its impact is just as significant.
It’s important for both patients and their healthcare providers to address these disruptions head-on. Strategies that manage fatigue must be multifaceted and adapted to each individual’s needs, including pain management, building healthy sleep habits, encouraging physical activity, and supporting mental health to break the cycle of daily exhaustion.
Sleep Quality, Fatigue, and Osteoarthritis
One of the most overlooked connections in OA management is the powerful relationship between sleep quality and fatigue. Many OA patients report difficulty falling or staying asleep due to pain or discomfort. This sleep disturbance prevents restorative rest, exacerbating both pain and daytime tiredness. Over time, even mild, recurring sleep disruption can lead to chronic arthritis fatigue, reduced resilience, and a downward spiral in overall quality of life.
Addressing sleep habits and prioritizing sleep quality are therefore essential in efforts to manage fatigue and improve physical function in osteoarthritis patients. Good sleep hygiene—such as keeping a regular bedtime, creating a soothing sleep environment, and seeking help for sleep disorders—can make a meaningful difference to sleep quality and, in turn, help patients reclaim more energy for daily life.
Impact of Sleep Problems on Fatigue
Sleep problems are a well-documented contributor to fatigue in OA. From sleep disturbance caused by pain to secondary conditions like insomnia, research has shown that people with OA have a higher likelihood of poor sleep and persistently low energy. This is partly due to the fact that pain tends to worsen at night, preventing patients from reaching the deep stages of sleep needed for physical and psychological recovery.
The result is not just a temporary feeling of being tired but a profound energy deficit that affects cognitive performance, mood, and the ability to cope with pain the next day. Over time, repeated cycles of poor sleep and pain reduce physical function, create more disease activity, and may even increase inflammation—compounding the mechanisms that cause fatigue in OA. For patients struggling with night pain and sleeplessness, targeted sleep interventions should be seen as an important facet of OA treatment.

Improving Sleep for Better Quality of Life
Improving sleep quality offers patients with OA one of the most effective ways to manage fatigue and enhance overall wellbeing. Establishing healthy sleep habits such as going to bed at the same time each night, using supports or pillows to alleviate joint discomfort, and limiting caffeine or blue light before bed can make a substantial difference. In cases where sleep problems persist, medical consultation may reveal treatable sleep disorders or indicate the need for medication adjustment to reduce night pain as a side effect.
With better sleep often comes increased daytime energy, better mood, reduced pain, and marked improvements in physical function and participation in daily life. For OA patients, these incremental improvements can combine to provide much-needed relief and re-open the door to a happier, fuller quality of life.
Table: Common Sleep Problems in Osteoarthritis and Practical Solutions
Sleep Problem |
How It's Related to OA |
Practical Solutions |
|---|---|---|
Nighttime pain/stiffness |
Pain and joint discomfort disrupt sleep cycles |
Use joint supports, pain medication before bed, adjust sleeping position |
Restless legs |
Pain and poor physical function trigger restless movements |
Stretching, warm baths, low-impact evening activity |
Frequent waking |
Pain flares or need to adjust position cause awakenings |
Mattress/pillow adjustment, timed pain medication, consult provider for sleep meds |
Insomnia |
Stress, anxiety, and pain related to OA |
Relaxation techniques, breathing exercises, cognitive behavioral therapy |
Does Knee Osteoarthritis Cause More Fatigue? Specifics and Research
While all forms of OA can drain energy, knee osteoarthritis tends to have a particularly large impact on fatigue due to the high load these joints bear in everyday movement. Studies comparing knee osteoarthritis to OA in other areas (like hands or spine) show that knee pain is more likely to cause physical function impairment, trigger frequent disease flares, and lead to significant reductions in quality of life—all contributing to greater fatigue in OA patients.
Compared to healthy individuals or those with other health conditions, people suffering from knee OA typically report higher fatigue levels, especially when pain is severe or sleep is disrupted. Understanding these risks allows for targeted interventions—such as physical therapy, exercise, and better pain control—aimed at improving daily energy and enabling continued mobility.
Knee Osteoarthritis, Pain Severity, and Physical Function
Knee osteoarthritis often leads to a significant drop in physical function, which directly impacts daily life energy levels and independence, contributing to greater fatigue. The combination of swelling, instability, and severe pain can make it difficult to walk, climb stairs, or even get out of a chair. This in turn leads to muscle weakening, further fatigue, and increased risk of falls and additional injury. According to research, fatigue levels in knee OA patients correlate closely with pain severity: the more intense the pain, the more profound and persistent the fatigue.
Addressing knee OA means more than just managing pain—it requires comprehensive strategies to support joint health, maintain physical function, and address all aspects of daily life. Rehabilitation exercises, strengthening programs, joint supports, and medical interventions should all be considered essential tools in reducing the overwhelming fatigue caused by knee osteoarthritis.
Comparison with Other Health Conditions like Rheumatoid Arthritis
Osteoarthritis is often compared to rheumatoid arthritis (RA), another chronic disease with a reputation for causing fatigue. While RA is driven primarily by autoimmune inflammation, both diseases produce similar symptoms, including pain, poor sleep, reduced physical function, and high levels of fatigue. Interestingly, research shows that the drivers of fatigue in OA (joint damage, mechanical pain, and lifestyle factors) overlap considerably with those in RA, though autoimmune disease activity and systemic inflammation are generally more pronounced in the latter.
Regardless of the specific health condition, the relationship between fatigue and chronic disease is clear—pain and inflammation heighten the feeling of exhaustion, while emotional health (including pain and depression) further drains resources. Recognizing these commonalities can help both patients and clinicians approach fatigue in a truly holistic way.
"Pain, stiffness, and poor sleep form a vicious cycle, leaving osteoarthritis sufferers persistently fatigued."
Pain and Depression: Dual Drivers of Fatigue in Osteoarthritis
Alongside chronic pain, depression is a major predictor of ongoing fatigue in OA patients. Both symptoms feed into each other: chronic pain increases the risk of depression, and depression, in turn, amplifies pain perception and reduces motivation to engage in health-promoting behaviors like exercise or social activities. The combined load of pain and mood changes creates a near-constant energy drain that’s hard to overcome without targeted treatment.
It’s important for patients to recognize that seeking help for depression is not a sign of weakness, but a crucial aspect of managing the side effects of OA, improving quality of life, and breaking the cycle of fatigue. Mental health support—whether through counseling, medication, or peer support groups—should be considered just as essential as physical therapy or pain medications in effective OA care.

How Depression and Chronic Pain Interact
Pain and depression have a complex, bi-directional relationship. Patients with more severe and persistent pain often develop depressive symptoms, which intensify feelings of helplessness, sadness, or loss of interest in daily life activities. Depression also lowers pain tolerance and disrupts sleep—a combination that drives ever-higher fatigue levels. For some, the psychological burden of OA is as profound as the physical limitations, making comprehensive treatment including mental health care a necessity, not an option.
Recognizing depression and chronic pain as integrated causes of fatigue allows for a more empathetic, individualized care approach. Managing both symptoms often results in rapid improvements in sleep, energy, and physical function, reaffirming the mind-body connection at the heart of OA management.
Maintaining Quality of Life Despite Side Effects
Despite the many side effects linked to OA—including fatigue, pain, and depression—patients can take practical steps to maintain or even improve their overall quality of life. This often means reimagining routines, seeking support, and using medical and lifestyle tools in combination. Integrating social connection, enjoyable activities, gentle exercise, and open communication with care teams can help ease the burden of fatigue in OA and restore a sense of control over the future.
By understanding these challenges and proactively seeking solutions, people with osteoarthritis can manage fatigue, maintain hope, and reclaim as much of their daily life as possible.
Managing Fatigue with Osteoarthritis: Tips, Treatments, and Lifestyle Changes
Successfully managing fatigue in OA requires a well-rounded approach—addressing chronic pain, improving sleep quality, maintaining physical function, and supporting emotional health to enhance overall quality of life. The following tips and strategies aim to tackle each contributing factor, fostering better quality of life and increased independence.
Whether you’re newly diagnosed or have lived with OA for years, these actionable steps can serve as a roadmap to manage fatigue and mitigate its most disruptive effects.
Lifestyle Strategies to Manage Fatigue
Simple lifestyle adjustments go a long way in managing arthritis fatigue. Stick to a consistent sleep schedule, limit caffeine, use relaxation techniques, and prioritize activities that bring joy or reduce stress. Pacing is key—alternating strenuous activities with periods of rest can prevent overexertion and lower fatigue levels. Seeking out community resources, such as peer support groups or occupational therapy, can also help identify ways to manage daily tasks more comfortably.
Meal choices matter, too. Following a balanced, anti-inflammatory diet may address underlying inflammation and provide the essential nutrients your body needs to stay resilient against OA’s daily demands.
Medical Management and Side Effects to Consider
Consult with your doctor about pain medications, physical therapy, or injections that may help control pain and inflammation. Be proactive about monitoring medication side effects, as some drugs used for OA may worsen fatigue. Never start, stop, or adjust medications without medical supervision. Additionally, talk to your care team about sleep aids or non-pharmacologic interventions if sleep problems become overwhelming.
Mental health support in the form of counseling or prescribed antidepressants can play a crucial role in treating underlying depression, further lowering fatigue levels and helping patients regain control over daily life.
Physical Activity for Physical Function and Fatigue Reduction
Regular, low-impact exercise is one of the most effective tools for minimizing fatigue in OA while rebuilding physical function. Gentle movement—walking, swimming, cycling, or yoga—can help keep joints flexible, maintain muscle mass, and boost mood. Even brief periods of daily movement make a difference; the key is consistency and avoiding over-exertion.
Physical therapists can design customized exercise programs tailored to your specific limitations and needs. The goal is to increase endurance, restore confidence, and improve energy for tackling daily tasks.

Maintain a regular sleep schedule
Consider low-impact exercise
Address pain with medication or therapy
Seek professional mental health support if needed
Monitor diet for anti-inflammatory effects
Can osteoarthritis make you feel very tired?
Answer: Yes, osteoarthritis can make you feel extremely tired due to chronic pain, sleep problems, and the disease's impact on both the body and mind.
The combination of constant pain, disrupted sleep quality, and psychological effects means OA can cause a level of fatigue that is often severe and not improved by ordinary rest. This symptom is now recognized as a key feature of the disease, on par with pain and stiffness.
What causes osteoarthritis to flare up?
Answer: Flare-ups can be triggered by increased physical activity, joint overuse, weather changes, or stress—leading to worsened pain and fatigue.
Any factor that raises disease activity—such as overuse or major changes in weather—can trigger flares in OA. During flares, patients often report higher pain, stiffness, swelling, and a sharp spike in fatigue levels. Managing these triggers with pacing, rest, and proactive care is essential for minimizing the impact on daily life.
What are the four stages of osteoarthritis?
Answer: The four stages include minor, mild, moderate, and severe, each with progressive joint damage and symptom severity, often including greater fatigue.
As OA progresses—from minor to severe—the symptoms intensify. Early stages may include brief joint stiffness or slight pain, while advanced stages bring chronic pain, joint deformity, and major loss of physical function. Fatigue in OA often increases alongside the worsening disease stage, making energy management more crucial as OA advances.
What is the diet for osteoarthritis?
Answer: A diet rich in anti-inflammatory foods—like fruits, vegetables, omega-3 fatty acids, and whole grains—may help manage both osteoarthritis symptoms and fatigue.
A healthy OA diet emphasizes fresh produce, fatty fish (such as salmon), nuts, seeds, and olive oil while reducing processed foods and added sugars. These choices can help lower systemic inflammation—a major contributing factor in OA flares and overall fatigue. Always discuss major dietary changes with your healthcare team to ensure the plan fits your specific health needs.

FAQs on Does Osteoarthritis Cause Fatigue
Are fatigue symptoms different in knee osteoarthritis versus other joints?
While fatigue can affect OA in any joint, studies indicate that knee osteoarthritis causes greater fatigue due to higher pain levels and more significant reductions in physical function. The energy demand for walking, standing, and daily mobility means that knee OA can be particularly draining.Can improving sleep quality significantly reduce fatigue caused by osteoarthritis?
Yes, improving sleep quality can lead to noticeable reductions in daytime fatigue. Targeted interventions—such as sleep hygiene routines, physical supports, or pain management—can break the cycle of poor sleep and persistent tiredness in OA patients.How do pain and depression combine to worsen tiredness in osteoarthritis?
Pain and depression often occur together in OA, each magnifying the other. This dual burden heightens fatigue by lowering energy, disrupting sleep, and eroding motivation—a cycle that can only be broken with holistic treatment addressing both body and mind.Are there medications specifically for fatigue in osteoarthritis?
While no drugs specifically target fatigue in OA, addressing underlying contributors (like pain, inflammation, or sleep problems) with medications can indirectly reduce fatigue. Always discuss medication choices and potential side effects with your doctor.What role does inflammation play in osteoarthritis-related fatigue?
Inflammation, both local and systemic, is a major factor in the fatigue experienced by OA patients. Ongoing inflammation taxes the immune system, interferes with sleep, and drains physical energy—making fatigue management a multi-pronged effort.
Key Takeaways on Does Osteoarthritis Cause Fatigue
Osteoarthritis can lead to pronounced fatigue due to pain, inflammation, and sleep disruption.
Addressing sleep quality and pain may improve daily energy and quality of life.
Dietary and lifestyle strategies are crucial for managing osteoarthritis fatigue.
Conclusion: Proactively Manage Fatigue to Improve Quality of Life with Osteoarthritis
By understanding the many ways OA triggers fatigue and using tailored management strategies, you can regain control, boost energy, and enjoy a better quality of life—even with osteoarthritis.
If you’re interested in learning how other chronic health conditions can impact daily living and what it takes to reclaim your vitality, you might find inspiration in stories of resilience and medical breakthroughs. Discover how a successful kidney transplant transformed one musician’s life and offered new hope for overcoming the challenges of chronic illness by reading this in-depth look at the impact of a successful kidney transplant. Exploring these journeys can provide valuable perspective and motivation as you navigate your own path to better health and energy.
Fatigue is a common and often debilitating symptom for individuals with osteoarthritis (OA). This persistent exhaustion can significantly impact daily activities and overall quality of life.
Understanding the Connection Between Osteoarthritis and Fatigue
Research indicates that fatigue in OA patients is multifaceted, influenced by several interrelated factors:
Chronic Pain: Persistent joint pain can be mentally and physically draining, leading to increased fatigue. (verywellhealth.com)
Sleep Disturbances: Pain and discomfort often disrupt sleep patterns, resulting in poor sleep quality and subsequent daytime fatigue. (belmarrahealth.com)
Inflammation: Ongoing inflammation associated with OA can contribute to feelings of tiredness and low energy levels. (homeinstead.co.uk)
Emotional Distress: The challenges of managing a chronic condition like OA can lead to stress, anxiety, and depression, all of which are linked to increased fatigue. (arthritis.org.au)
Managing Fatigue in Osteoarthritis
Addressing fatigue requires a comprehensive approach:
Pain Management: Effective control of joint pain through medications, physical therapy, or other interventions can help reduce fatigue. (medicalnewstoday.com)
Improving Sleep Quality: Establishing good sleep hygiene practices, such as maintaining a regular sleep schedule and creating a comfortable sleep environment, can enhance restfulness. (belmarrahealth.com)
Regular Physical Activity: Engaging in low-impact exercises like walking or swimming can improve joint function and reduce fatigue. (arthritis.org)
Stress Reduction: Techniques such as mindfulness, meditation, or counseling can help manage emotional stress and alleviate fatigue. (arthritis.org.au)
By understanding the link between osteoarthritis and fatigue, individuals can implement strategies to manage their symptoms and improve their quality of life.
For More Health & Wellness, visit: https://ncwellnesshub.com/
 Add Row
Add Row  Add
Add 



Write A Comment