Did you know that ignoring osteoarthritis and cartilage damage can lead to irreversible joint pain and mobility loss? Understanding these conditions now can help protect your future health and keep you moving freely.

Are you ready to learn how to safeguard your joints effectively? Read on for an in-depth, practical, and personal perspective on why osteoarthritis and cartilage issues demand your attention—and proactive action.
Osteoarthritis and Cartilage: Understanding the Fundamentals
When discussing osteoarthritis and cartilage, it’s crucial to start with a strong foundation in what these terms truly mean and why open access to research in this field can be transformative. Osteoarthritis is one of the most widespread chronic joint conditions worldwide, impacting millions and leading to joint pain and reduced mobility. Cartilage, often overlooked, is central to joint function—it cushions the bones, supports smooth movement, and bears the brunt of daily mechanical stress. Without healthy cartilage, even simple movements can become agonizing, and joint function severely impaired.
The significance of understanding cartilage open access journals and their freely available research cannot be overstated. It fosters a collaborative environment for sharing research breakthroughs and treatment protocols freely with practitioners, researchers, and patients. Journals such as the official journal of the Osteoarthritis Research Society International (OARSI) are pivotal in disseminating information across disciplines involved in osteoarthritis research.
Open access journal articles provide unrestricted information to all, ensuring that new therapies and clinical insights are not confined behind paywalls. This mutual sharing of experimental or clinical studies empowers multidisciplinary teams to make advances faster and gives patients real hope through knowledge.

What is Osteoarthritis and Cartilage Open Access?
Osteoarthritis is a degenerative joint condition marked by the gradual breakdown of cartilage, leading to pain, stiffness, and functional impairment. Open access in this context refers to freely available scientific literature on osteoarthritis and cartilage conditions that can be accessed by anyone, anywhere, without a subscription. Open access journals play a vital role—they accelerate the spread of experimental or clinical studies, study protocols, and the latest findings.
This transparency in research enhances global understanding and equips both specialists and practitioners concerned with osteoarthritis with the latest science, fostering more rapid progress in the field. For patients, open access provides a trusted source for empowering themselves with information about their conditions and care options.
Cartilage Function: The Unsung Hero of Joint Health
Cartilage is often called the silent workhorse of the joints—a resilient, flexible tissue that covers and cushions the surfaces where bones meet. Functionally, it acts like a shock absorber during movement, allowing for smooth, pain-free motion and protecting bones from damaging friction. When cartilage open research is widely shared, practitioners gain better insights into how cartilage failure leads to conditions like osteoarthritis, and how cartilage regeneration might work.
In fact, the multidisciplinary journals that disseminate information about cartilage help bridge fields from orthopedics to molecular biology. They facilitate communication between kinds of specialists, from experimental stem cell researchers to frontline clinicians. When healthy, cartilage lets us run, jump, and live actively; when damaged, its breakdown is often irreversible, leading to pain and long-term disability.
For those interested in how osteoarthritis and cartilage damage compare to other joint conditions, exploring the broader landscape of arthritis types can provide valuable context. Understanding the distinctions between osteoarthritis and other forms of arthritis helps clarify why early intervention and targeted care are so important for joint health. Discover more about the diverse world of arthritis types and how they impact the body.
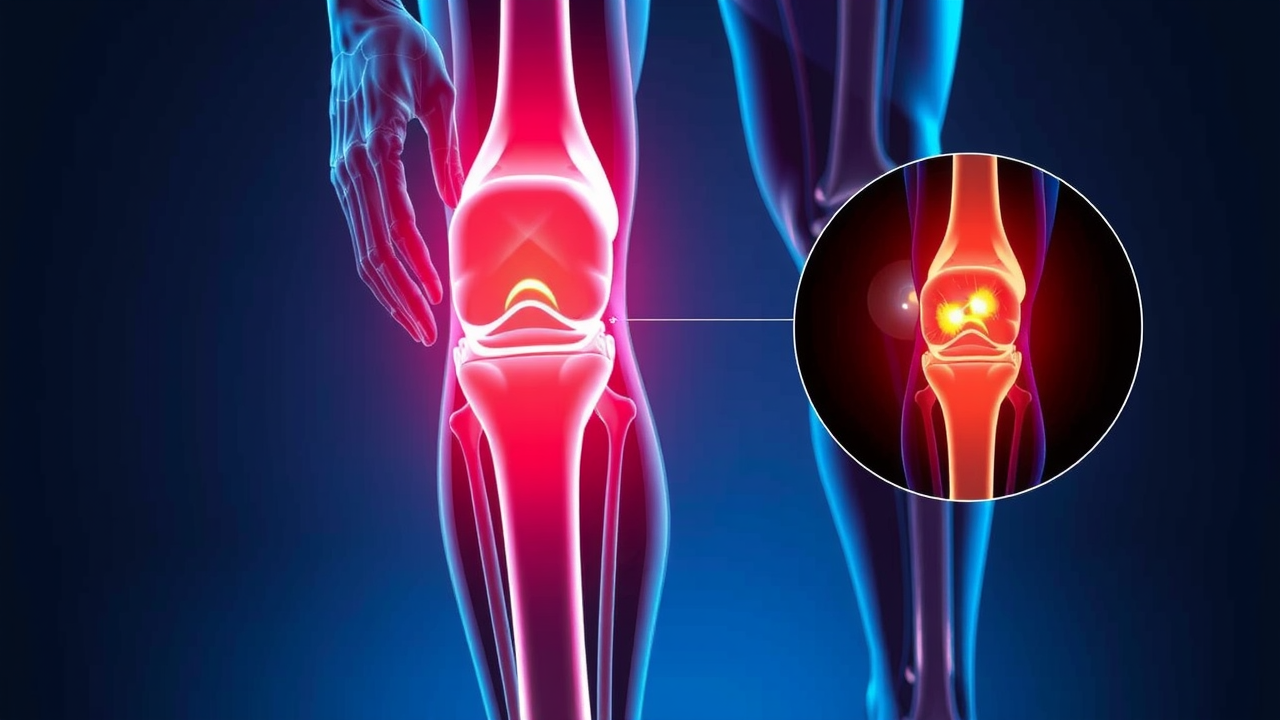
The Vital Link Between Osteoarthritis and Cartilage Damage
The relationship between osteoarthritis and cartilage damage is both direct and devastating, as highlighted in numerous osteoarthritis and cartilage open access studies. Osteoarthritis can’t occur without some element of cartilage breakdown—meaning your joint health hinges on this thin layer of tissue. Cartilage acts as a cushion and provides a smooth surface, but osteoarthritis attacks it slowly and relentlessly.
With the accelerating pace of research society international collaborations, we're learning just how early cartilage damage starts before symptoms appear, and how quickly the condition can progress if ignored. The information obtained from experimental or clinical studies and sets obtained from open access journals gives clinicians critical clues for early interventions.
The deterioration of cartilage sets off a cascade: bone starts to rub on bone, inflammation ramps up, and new growth (osteophytes or bone spurs) begins to deform the joint. Over time, cartilage breakdown becomes the main culprit behind loss of mobility and chronic pain, restricting daily activities or even leading to joint replacements. This connection is the reason the Journal of the Osteoarthritis Research Society International and similar organizations champion awareness—highlighting how essential it is to diagnose and manage osteoarthritis and cartilage disorders early. The link is so fundamental that practitioners concerned with osteoarthritis almost always direct their first attention to the status of the cartilage in affected joints.
How Osteoarthritis Damages Cartilage Open Access
Osteoarthritis damages cartilage in a gradual, progressive manner. It starts with minor surface cracks and fibrillation, which may not cause immediate pain or obvious symptoms. As the process continues, these cracks deepen and the cartilage thins, losing its buoyant, cushioning properties. Osteoarthritis and cartilage open access research studies have repeatedly proven that as cartilage volume decreases, the friction inside the joint increases.
This not only accelerates the wear and tear but also triggers the inflammatory response, exacerbating swelling and discomfort. Numerous multidisciplinary journals that disseminate information about these microscopic processes help specialists recognize subtle changes and develop early intervention strategies before permanent joint damage occurs.
Furthermore, open access publications are invaluable for understanding how genetics, immune responses, lifestyle choices, and even certain medications interact to accelerate cartilage loss. These mechanisms are not just theoretical: they inform the latest study protocols and direct clinical decision-making. This is why journals—especially those obtained from experimental work—are so vital for practitioners and the wider community interested in halting the progression of osteoarthritis and cartilage degeneration.
Progression: From Initial Symptoms to Advanced Cartilage Breakdown
Osteoarthritis is notorious for its slow and insidious onset. Initially, a person may feel mild joint stiffness or transient aches after activity, often dismissed as the effects of aging or overuse. However, as osteoarthritis and cartilage damage sets in, these symptoms intensify. Cartilage begins losing its smooth, glass-like texture, becoming rough and fragmented. This transition brings about persistent pain, swelling, and reduced mobility. While the timeline varies, without intervention, cartilage may erode entirely, leaving bones exposed and causing the characteristic ‘grinding’ sensations of advanced disease.
Clinical and experimental studies outlined in official, open access journals highlight how critical the early stages are for prevention and treatment. The presence of biomarkers, imaging changes, and even genetic predispositions are all covered in detail in the multidisciplinary journals that disseminate this information.
As damage progresses, other joint tissues—like the bone just beneath the cartilage and structures such as the intervertebral disc—are affected, amplifying pain and disability. The key lesson is that early attention to even minor symptoms can halt or slow the relentless slide from mild discomfort to severe, life-altering limitations.
Why You Shouldn’t Ignore Osteoarthritis and Cartilage Problems
Ignoring osteoarthritis and cartilage damage isn’t just about tolerating pain. These conditions can profoundly affect every aspect of your life, from basic mobility to independence, and even your psychological well-being. The persistent joint pain of osteoarthritis is more than a nuisance—it’s a harbinger of escalating issues, including compromised movement, increased fall risk, and long-term health complications such as weight gain, muscle loss, and cardiovascular decline due to reduced activity. The danger is that untreated cartilage damage doesn’t stay static; it gets worse, often rapidly once symptoms accumulate, locking you into a vicious cycle of pain and inactivity.
Healthcare practitioners concerned with osteoarthritis emphasize that timely recognition and treatment are essential for preserving joint health. As the research society international and open access journal articles continually stress, early management can prevent irreversible damage. Most multidisciplinary journals that disseminate information on this topic advocate not just for medical therapies, but also for lifestyle modifications and holistic approaches. The bottom line is clear: waiting to address joint pain or stiffness until “it’s bad enough” can mean missing the ideal window for intervention—and a dramatically worse prognosis.

Pain, Mobility Loss, and Long-term Health Risks
One of the most immediate and distressing consequences of osteoarthritis and cartilage disorders is joint pain. This pain doesn’t just limit movement; over time, it discourages activity, leads to muscle atrophy, and decreases your overall quality of life. Long-term, loss of mobility can set off a domino effect, causing other health risks such as obesity, diabetes, and even depression. In severe cases, untreated cartilage loss can result in permanent joint deformity or necessitate invasive surgeries like joint replacements.
"Ignoring osteoarthritis and cartilage damage is like letting rust eat away at the engine of your body—eventually, things will grind to a halt."
The impact isn’t only physical: it can alter social life, employment, and emotional health. Early intervention is consistently recommended in official journals and by international research societies. The sooner joint pain and mobility loss are addressed, the more positive the long-term outlook becomes, navigating away from disability and dependence.
Open Access to Research: A New Era for Osteoarthritis and Cartilage Treatments
Open access publishing has revolutionized the way information about osteoarthritis and cartilage is disseminated to researchers and clinicians worldwide. Journals dedicated to open access, such as the Osteoarthritis and Cartilage Open, have made the latest research and clinical insights available to the public, researchers, and practitioners without financial barriers. This democratization of knowledge is crucial—patients can self-educate, and clinicians can keep up with rapidly evolving therapies that can dramatically improve joint health outcomes.
The beauty of open access is in its inclusivity: it draws on the expertise of specialists and practitioners concerned with osteoarthritis from every part of the globe. Access journals encourage submission of everything from study protocols to comprehensive review articles, expanding the collective knowledge base. The more multidisciplinary the journal, the more kinds of specialists can contribute, ensuring that treatments continue to advance and reach those who need them most. The result? A significant leap forward in the speed and applicability of osteoarthritis and cartilage research across all settings.

How Open Access Empowers Patients and Professionals
Open access journals empower both patients and medical professionals to stay informed about the latest breakthroughs in osteoarthritis and cartilage open research. For patients, this means understandable, up-to-date resources on new therapies, rehabilitation strategies, and preventative interventions. For professionals, open access journals present peer-reviewed, experimental or clinical studies, and guidelines needed to make evidence-based decisions. The Osteoarthritis Research Society International, among others, backs this approach as the key way for practitioners concerned with osteoarthritis to remain at the leading edge of care. Open access literally bridges the gap between scientific discovery and real-world patient outcomes—transforming information obtained from experimental settings into treatment realities for all.
This collaborative model has encouraged participation from a variety of disciplines involved in joint health, including biologists, physiotherapists, orthopedic surgeons, and patient advocates. When a multidisciplinary journal that disseminates information operates without access restrictions, it ensures the reach and impact of its findings are maximized. The benefits to public health are clear and far-reaching, as new protocols and research can be swiftly shared and implemented.
Summary of Open Access Journals and Key Osteoarthritis and Cartilage Research Findings
Journal Name |
Focus Area |
Recent Breakthroughs |
Accessibility |
|---|---|---|---|
Osteoarthritis and Cartilage Open |
Comprehensive studies on joint degeneration and therapy development |
Novel cartilage regeneration methods, early diagnostic imaging protocols |
Free to access worldwide |
Osteoarthritis Research Society International Journal |
Interdisciplinary research and consensus treatment guidelines |
Global registries tracking long-term joint outcomes, patient-centered care data |
Accessible with open access options |
Cartilage |
Basic science and clinical translate studies |
Advancements in tissue engineering, stem cell treatments |
Hybrid; select articles open access |
Modern Treatments for Osteoarthritis and Cartilage Repair
The landscape of osteoarthritis and cartilage treatment is rapidly evolving, largely due to the dissemination of findings through open access journals and collaborative osteoarthritis and cartilage open research initiatives. Gone are the days when painkillers and joint replacements were the only solutions available. Today, a wide range of therapies—from lifestyle management and regenerative medicine to minimally invasive surgeries—form the core of current care. Updated guidelines now emphasize not just symptom control but also joint preservation, improved mobility, and better quality of life through a combination of evidence-backed approaches.
The guidance provided in multidisciplinary journals that disseminate information globally has enabled professionals to tailor treatment plans to individual needs, considering factors such as age, activity level, joint health, and underlying causes of osteoarthritis. The accessibility of up-to-date, science-driven protocols means that even community practitioners can offer care grounded in the best available evidence, a far cry from one-size-fits-all approaches of the past.

Current Guidelines and Therapies
Treatment guidelines for osteoarthritis and cartilage focus on a multi-pronged approach. Early interventions often include lifestyle modifications, such as weight loss, dietary adjustments, and exercise programs tailored to the individual’s limitations and goals. Medications like NSAIDs (nonsteroidal anti-inflammatory drugs) are commonly used for pain relief and inflammation reduction. For more advanced cases, physical therapy plays a central role—restoring strength, mobility, and confidence in joint use.
When conservative methods are insufficient, physicians might consider advanced therapies, including hyaluronic acid injections, platelet-rich plasma (PRP), or stem cell treatments. The availability of such therapies is frequently discussed in open access journals, with studies showing promising results in slowing cartilage loss and stimulating repair. In particular, experimental or clinical studies obtained from both human and animal models shed light on optimal candidates, dosing strategies, and long-term safety profiles. These ongoing findings are regularly disseminated by leaders in the osteoarthritis research society international community, keeping patients’ options open and up to date.
Cartilage Regeneration: What’s Possible Today?
One of the most exciting frontiers in osteoarthritis and cartilage care is the field of cartilage regeneration. Historically, cartilage was considered almost irreplaceable once damaged—but new advances in cellular engineering, biomaterials, and surgical techniques have begun to shift this paradigm. Research published in open access journals highlights techniques like microfracture surgery, autologous chondrocyte implantation, and tissue-engineered scaffolds designed to stimulate the body’s own healing response. For specific patients, especially those with focal cartilage defects, these interventions can restore some function and significantly reduce pain.
While full cartilage regeneration across extensive joint surfaces remains elusive, ongoing clinical trials and protocols described in access journals show steady progress. Stem cell therapies, for example, are under rigorous investigation, and bioprinting approaches are emerging as promising solutions. Practitioners concerned with osteoarthritis and those part of the research society international network are optimistic but emphasize the importance of setting realistic expectations—most regenerative approaches are either adjuncts to conventional therapy or reserved for select candidates. Nevertheless, the future for repairing osteoarthritis and cartilage damage is brighter than ever, thanks in large part to transparent, open access reporting of experimental outcomes.
-
Top 5 Emerging Treatments for Osteoarthritis and Cartilage Damage:
Platelet-Rich Plasma (PRP) Therapy: Uses concentrated platelets from the patient’s blood to encourage healing and reduce inflammation.
Biologic Injectables: Including stem cell therapies and growth factor injections showing promise in regenerating cartilage tissue.
Tissue Engineering and Scaffolding: Advanced biomaterial scaffolds provide frameworks for new cartilage cell growth in damaged joints.
Gene Therapy: Early studies focus on switching on cartilage repair genes within joint cells, aiming for long-term regeneration.
Minimally Invasive Surgical Techniques: Microfracture, mosaicplasty, autologous chondrocyte implantation, and related approaches designed to repair or replace small areas of cartilage damage, promoting improved joint function.

The Author’s Perspective: Why Public Awareness Matters
Despite the high prevalence and impact of osteoarthritis and cartilage conditions, public understanding remains limited, underscoring the need for greater access to osteoarthritis and cartilage open research. From my experience as a patient advocate and health communicator, it’s clear that raising awareness isn’t just about education—it’s a form of prevention.
Too often, people dismiss early joint pain as a minor inconvenience or inevitable aspect of aging, missing the critical moments when intervention makes the biggest difference. Working with the Osteoarthritis Research Society International and reading numerous open access journal articles, I have seen firsthand how knowledge shifts attitudes, resulting in swifter diagnoses and improved outcomes for countless individuals.
Society’s underestimation of osteoarthritis and cartilage open issues can perpetuate a cycle of inaction, leading to more advanced disease and higher healthcare costs. Recognizing the early signs, understanding risk factors, and breaking through stigma around “wear and tear” conditions are key steps. As the body of research grows and more people access quality information, I am hopeful for a future in which fewer people suffer unnecessarily from these entirely manageable conditions.
Society’s Perception of Osteoarthritis and Cartilage Conditions
The prevailing public view of osteoarthritis is that it’s a “natural” part of getting older—something inevitable, beyond personal control, or not worthy of serious concern. This perception is misguided and dangerous, as it delays help-seeking behaviors and diminishes investment in prevention. As outlined in many open access journals and multidisciplinary sources, early detection and lifestyle modification can profoundly impact disease progression. When patients are empowered by information obtained from experimental or clinical studies, they can advocate for themselves and avoid piecemeal, reactionary care.
Additionally, the public often overlooks the role of cartilage health in athletic or workplace injuries—believing that only seniors are at risk. Yet, osteoarthritis and cartilage damage are showing up in younger populations due to sports injuries and lifestyle changes. Raising awareness through channels like the journal of osteoarthritis research and supporting society international campaigns is essential to change mindsets and enable proactive, preventative healthcare across all ages.
Barriers to Diagnosis and Treatment
Several obstacles contribute to the underdiagnosis and undertreatment of osteoarthritis and cartilage conditions. First, symptoms often begin mild and progress slowly, lulling individuals into complacency. Primary care providers may dismiss joint pain as temporary or normal, especially if the patient is under 50 or active. Second, not everyone has easy access to musculoskeletal specialists or advanced imaging—even when these are crucial for accurate diagnosis. Third, socioeconomic and cultural factors can stop people from seeking or adhering to recommended therapies or lifestyle changes.
"Timely intervention can mean the difference between lifelong mobility and chronic disability."
These barriers can—and must—be addressed through education, accessible care paths, and the sharing of updated protocols from the latest journal that disseminates evidence-based practice. Open access is already leveling the playing field for practitioners, but a sustained effort is needed to ensure all patients understand when and how to seek help for osteoarthritis and cartilage issues.
People Also Ask About Osteoarthritis and Cartilage
What happens to cartilage in osteoarthritis?
In osteoarthritis and cartilage, the smooth cartilage surface wears down, leading to pain, friction, and restricted movement. The loss of cartilage exposes underlying bone and accelerates joint deterioration.
How do you stop osteoarthritis from progressing?
Managing osteoarthritis and cartilage damage involves lifestyle modifications, weight management, exercise, and medications that slow disease progression and protect joint health.
What is the best treatment for osteoarthritis?
The best treatments for osteoarthritis and cartilage issues depend on severity, from NSAIDs to physiotherapy, and sometimes surgical interventions.
What is the life expectancy of someone with osteoarthritis?
Osteoarthritis and cartilage disorders usually don’t affect overall life expectancy, but they can significantly impact quality of life and independence if not managed.

FAQs — Osteoarthritis and Cartilage
Can damaged cartilage heal on its own?
No, significant cartilage damage rarely heals on its own because cartilage has limited blood supply. Minor injuries might stabilize, but deep or extensive loss often requires medical intervention. Treatments such as physical therapy, biologic injections, or surgical procedures aim to halt further deterioration or stimulate repair, but prevention and early management are the most effective approaches.
Is osteoarthritis genetic or lifestyle-related?
Osteoarthritis and cartilage degeneration are influenced by both genetics and lifestyle. Family history, age, and inherited structural joint differences can increase risk, while factors like joint injuries, obesity, and sedentary habits can accelerate the breakdown. By identifying personal risks, individuals can take proactive steps to minimize their chances of developing severe osteoarthritis.
Are there preventative measures for young adults?
Yes, young adults can take meaningful measures to protect their joints. Maintaining a healthy weight, staying physically active with joint-friendly exercises, wearing protective gear, and managing injuries promptly are all crucial. Regular check-ups and early attention to persistent joint pain or stiffness can allow for early intervention and reduce long-term risk of osteoarthritis and cartilage damage.
Key Takeaways: Why Osteoarthritis and Cartilage Health Matter
Early detection prevents disability: Prompt recognition and treatment of joint pain safeguard long-term mobility.
Protect your cartilage daily: Manage body weight, stay active, and avoid repetitive joint stress.
Knowledge is empowerment: Use open access resources to stay informed about advances in osteoarthritis and cartilage care.
Lifestyle choices matter: Balanced nutrition, physical activity, and injury prevention reduce the risk and progression.
Don’t delay intervention: Consult experts early if you notice symptoms—timely action makes all the difference.
Conclusion: Take Action for Your Osteoarthritis and Cartilage Health
Safeguard your joints—early intervention is key. Stay informed and proactive in your approach to osteoarthritis and cartilage care.
If you’re ready to take your understanding of joint health even further, consider exploring the full spectrum of arthritis conditions and how they differ from osteoarthritis. Gaining insight into the various types of arthritis can help you recognize early warning signs, appreciate the nuances of treatment, and make more informed decisions about your long-term well-being.
By broadening your knowledge, you empower yourself to advocate for the best possible care and prevention strategies. Delve into the diverse world of arthritis types and discover advanced approaches to joint health—your future mobility may depend on it.
Sources
Osteoarthritis and Cartilage Journal – https://www.oarsijournal.com/
Osteoarthritis Research Society International – https://www.oarsi.org/
NIH Osteoarthritis Research – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7401170/
Understanding the intricacies of osteoarthritis and cartilage health is crucial for effective management and prevention. The Mayo Clinic’s article, “Osteoarthritis - Symptoms & causes,” provides a comprehensive overview of the condition, detailing its symptoms, causes, and risk factors.
Additionally, the National Institute of Arthritis and Musculoskeletal and Skin Diseases offers valuable insights in their piece, “Osteoarthritis Symptoms, Causes & Risk Factors,” which delves into the disease’s progression and its impact on joint health. If you’re serious about safeguarding your joints and understanding osteoarthritis, these resources will equip you with essential knowledge and strategies.
 Add Row
Add Row  Add
Add 



Write A Comment